This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Mental stress linked to increased heart risks in heart disease patients
Imagine walking through a park and suddenly spotting a bear. Normally your heart starts beating faster and your blood vessels constrict. That's the sympathetic nervous system preparing your body for a "flight or fight" response. Then, once you reach safety, your parasympathetic nervous system helps calm you down. Eventually, your blood pressure and heart rate return to normal.
For some people with heart disease, however, this experience can be concerning because stressful events can further negatively impact the heart. In 2021, NIH-supported researchers found that one in six people with heart disease were twice as likely to experience myocardial ischemia—a reduction in blood flow to the heart—when they experienced mental stress and that, in turn, was linked to increased risks for having a heart attack or a heart-related death years later.
Now, the same researchers have identified a key mechanism involved. Their findings, published in Circulation: Cardiovascular Imaging, homed in on the parasympathetic and sympathetic nervous systems, which help the brain communicate with the heart, and found that a dysregulated response, measured by reductions in heart rate variability (the variation in time between two heartbeats) appears to influence this increased risk for ischemia.
The findings are helping researchers understand what's happening beneath the surface for people with coronary artery disease who experience mental stress-induced ischemia, said Rebecca Campo, Ph.D., a program officer in the Clinical Applications and Prevention branch in the Division of Cardiovascular Sciences at the National Heart, Lung, and Blood Institute (NHLBI). "Generally, a healthy response to stress is when the sympathetic and parasympathetic nervous systems work in harmony ," she explained.
Campo noted that like a teeter-totter during mental stress, the sympathetic nervous system kicks in, while the parasympathetic nervous system withdraws. This flops when the parasympathetic response is activated and soothes physiological responses to stress. Lower heart rate variability may reflect dysfunction in these two systems and a state where the sympathetic nervous system is more dominant.
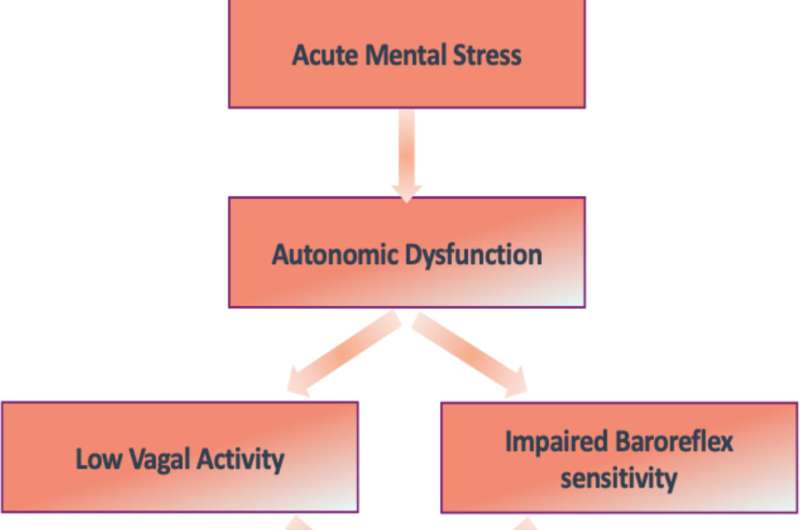
The researchers suspected that an imbalance between the two systems, also called autonomic dysregulation, is what may lead to mental stress-induced ischemia. To evaluate this, they measured heart rate variability to see if they could pinpoint the connection.
When the time between heart beats fluctuates a lot, they knew, it often translates to a person's ability to quickly sense and respond to stress. In other words, this signals that their autonomic nervous system is adaptive. If the time between beats doesn't change much, this suggests there could be problems.
To test this in the lab, the researchers evaluated cardiovascular outcomes from more than 700 adults who participated in the Myocardial Infarction and Mental Stress Study 2 and the Mental Stress Ischemia Mechanisms and Prognosis Study.
Participants fasted overnight and were asked to rest 30 minutes before the start of the exercise. They were then assigned a standard laboratory mental stress-inducing task: to prepare a speech envisioning how they would respond to learning about the mistreatment of a loved one in a senior living facility. They had two minutes to prepare the speech and three minutes to deliver it in front of at least three people.
The participants wore portable heart monitors to measure their heart rate variability in five-minute increments before, during, and after the task. They also had cardiac imaging track their heart's activity and blood flow during rest and the mental stress task.
The findings confirmed the research team's hypothesis. During the mental stress test, 119 participants, 16% of the study sample, experienced myocardial ischemia. Those with the lowest heart rate variability, which signaled a poor cardiovascular response to stress, accounted for about one-fourth of study participants. The researchers found these participants were twice as likely to experience ischemia during the mental stress challenge compared to those with higher heart rate variability.
Amit J. Shah, M.D., a cardiologist at the Atlanta VA Medical Center, an associate professor of epidemiology at Emory University's Rollins School of Public Health, and the lead study author, said many reasons could explain responses to mental stress. A weak heart—which could have resulted from a major heart attack—is one of them.
That's because the heart plays as much of a role as the brain in the functioning of the autonomic system, Shah said. "Both are voting members in terms of what happens with heart rate variability," he added.
Participants also completed a conventional stress test, which included walking on a treadmill until they reached their maximum heart rate. This type of physical stress did not elicit the same response as the speech exercise—reinforcing that mental stress activates distinct physiological responses in the body.
Shah and his colleagues, including first study author Jeffery Osei, M.D., M.P.H., noted that more research is needed to pinpoint the specific pathways involved in how autonomic dysregulation causes mental stress-induced myocardial ischemia. However, findings from this study and future studies could help advance research focused on ways to minimize these effects and also support cardiovascular function.
For example, the researchers suggested that future studies could assess if wearable heart rate monitors may help people with heart disease recognize early signs of stress and take steps to offset risks for heart problems. Others may study the effectiveness of pairing early detection with interventions, such as aerobic exercise, yoga, deep-breathing exercises, or even medications for people with significant risks, to help the body better sense and respond to stress.
"The more we can do after stressful events to help replenish and restore our body's normal functions, such as through activating the parasympathetic nervous system, the better—and the more we'll be doing to help our hearts," said Campo.
This research was supported by grants from the National Institutes of Health, including NHLBI, the National Institutes of Mental Health, the National Institute of Minority Health and Health Disparities, and the National Center for Advancing Translational Sciences.
More information: Jeffery Osei et al, Stress-Induced Autonomic Dysfunction is Associated With Mental Stress–Induced Myocardial Ischemia in Patients With Coronary Artery Disease, Circulation: Cardiovascular Imaging (2024). DOI: 10.1161/CIRCIMAGING.124.016596




















