This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Bipolar disorder and alcohol: It's not as simple as 'self-medication,' says study
Bipolar disorder and alcohol problems seem to go hand-in-hand, leading to a widespread belief that drinking acts as a kind of "self-medication" to ease bipolar's life-altering symptoms of mania, depression, anxiety, sleep disturbances and more.
But a new study suggests a much more complex interaction between the two.
Using ten years of data from nearly 600 people with bipolar disorder who volunteered for a long-term University of Michigan study, researchers show that even short-term increases in drinking can have lasting effects, even among those who drink fewer drinks than experts consider problematic.
But the opposite wasn't true: those who experienced an uptick in their symptoms didn't go on to have increased drinking that would indicate self-medication. The study was published in JAMA Network Open.
The researchers, based at the Heinz C. Prechter Bipolar Research Program, say this can be important knowledge for people with bipolar disorder and for the clinicians involved in their care.
Whether they decide to drink or not, keeping alcohol consumption levels consistent and including discussions of drinking habits in mental health appointments could be key.
"Our study shows that when an individual with bipolar disorder drinks more than typical for them, regardless of how much more, they are more likely to show an increase in depressive and/or manic symptoms over the following six months, even if they did not have a co-occurring alcohol use disorder," says first author Sarah Sperry, Ph.D., a psychologist and assistant professor at Michigan Medicine's Department of Psychiatry who specializes in bipolar disorder care and research. "Contrary to the self-medication hypothesis, there was no evidence that having increased mood symptoms predicted lasting changes in alcohol use over the following six months."
Sperry notes that previous studies have shown that more than half of people who have a bipolar disorder diagnosis also experience alcohol use disorders sometime in their lives, and that many report using alcohol to help them get to sleep.
But few studies have explored the interaction between the two or sought to address them together.
Study volunteers' data makes a big difference
Thanks to the massive amounts of data available from the Prechter Longitudinal Study of Bipolar Disorder (PLS-BD), Sperry and her colleagues are making headway on understanding the interaction.
The PLS-BD is a unique and detailed longitudinal study that has engaged over 1,500 individuals with and without bipolar disorder who are helping scientists identify biological, genetic, psychological, and environmental causes of bipolar disorder and its trajectory over time. All of them completed measures of mood symptoms, life functioning, alcohol use and more every 2 months throughout their involvement in the study.
"This is exactly the type of data needed to test how mood symptoms impact an individual's alcohol use and conversely, how changes in alcohol use impact mood symptoms" says Sperry, the Prechter Program's associate director.
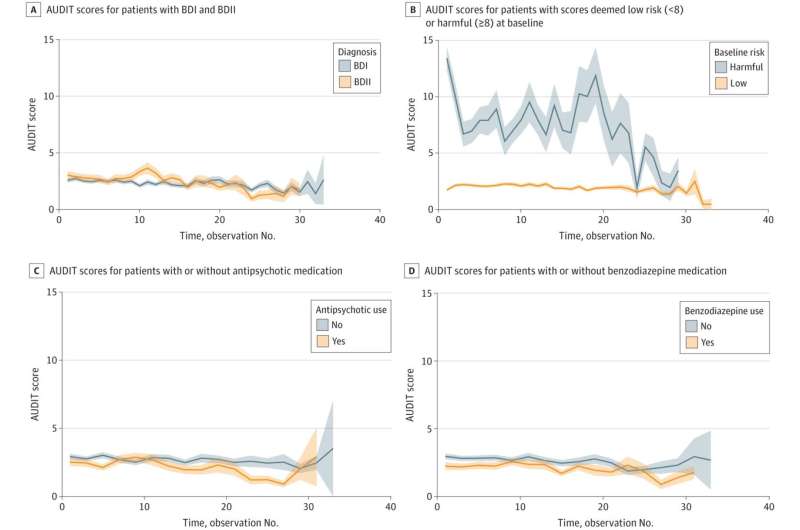
Using sophisticated computational approaches needed for this type of intensive longitudinal data, doctoral candidate Audrey Stromberg, Sperry and their collaborators examined the bi-directional relationships between alcohol use and mood symptoms over 10 years in 584 individuals with a bipolar disorder.
They also looked at the impact of alcohol use on functioning across domains of family, friend, work, and home life and found that drinking more than typical amounts of alcohol was linked with a higher likelihood of problems in work functioning over the following six months. This was true for individuals with both of the most common forms of the condition, called bipolar I disorder and bipolar II disorder, although it was even more pronounced in individuals with bipolar II disorder.
The findings were seen even in people who were not engaging in binge drinking, drinking with high intensity or frequency, or experiencing impairment related to their alcohol use. As a result, they suggest that clinics should use a standardized measurement tool such as the Alcohol Use Disorder Identification Test (AUDIT) to gauge alcohol use patterns at any level over time, and guide conversations between patients and providers.
Advice for today—research for tomorrow
Sperry and her team at her EmoTe Laboratory have already begun following up on the new findings to try to identify psychological and neurophysiological factors that contribute to alcohol use and symptom changes in bipolar disorder. Ultimately, they hope to develop new interventions that target both.
For now, the key message about alcohol use for people with bipolar disorder seems to be to keep things consistent over time—just like clinicians advise them to do with sleep schedules, medication schedules, and eating patterns.
For instance, patients who see alcohol as a tool to get to sleep or calm anxiety may be best off focusing on keeping their alcohol use low and stable, and avoid bingeing. Others may see the new findings as important for resisting peer pressure to binge drink during social situations. Findings may aid patients and their clinicians to have conversations about abstaining from alcohol vs. engaging in harm reduction strategies, Sperry notes.
"The reasons behind our findings likely have more to do with what alcohol and social situations involving alcohol do to a person's circadian rhythms and brain-based reward circuits, not just the action of the substance in the brain," says Sperry.
For instance, the brains of people with bipolar disorder may be more sensitive to disruptions in communications that alcohol can cause, and slower to recover from those impacts. Sperry and her colleagues are preparing to study this and other aspects of brain activity using EEG, or electroencephalogram, as well as mobile and wearable technologies to measure real-world behaviors.
They're currently enrolling participants for this new study. The Prechter Longitudinal Study is also still enrolling both people with bipolar disorder and people with no mental health conditions or close relatives who have mental health conditions, to act as comparisons.
More information: Sarah H. Sperry et al, Longitudinal Interplay Between Alcohol Use, Mood, and Functioning in Bipolar Spectrum Disorders, JAMA Network Open (2024). DOI: 10.1001/jamanetworkopen.2024.15295



















