This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Long-term cognitive and psychiatric effects of COVID-19 revealed in new study
Many people who were hospitalized with COVID-19 continue to have cognitive and psychiatric problems even two to three years post-infection, according to a study published in The Lancet Psychiatry, titled "Cognitive and psychiatric symptom trajectories 2-3 years post-COVID-19 hospitalization: a longitudinal prospective cohort study."
Conducted by a group of researchers across the UK led by the University of Oxford and the University of Leicester, the research highlights the persistent and significant nature of these symptoms as well as the emergence of new symptoms years after COVID-19 was first present.
The research was conducted with 475 participants (as part of the PHOSP-COVID study) who were invited to complete a set of cognitive tests via their computer and to report their symptoms of depression, anxiety, fatigue and their subjective perception of memory problems. They were also asked whether they had changed their occupation and why.
The researchers found:
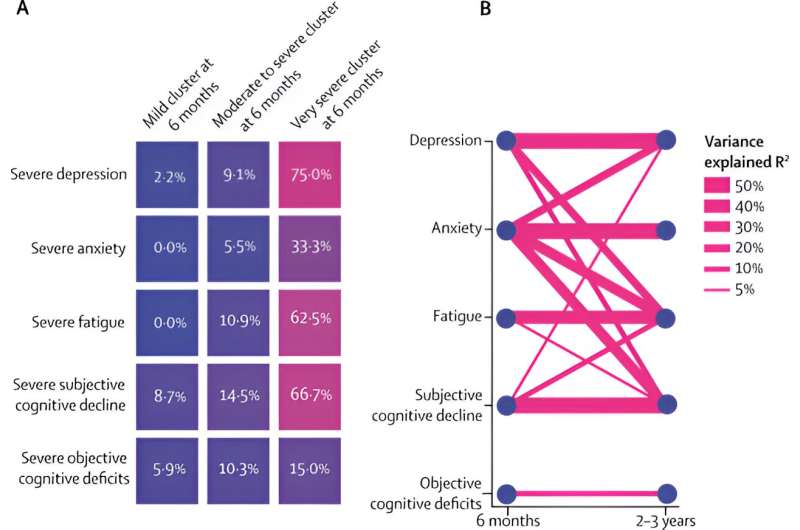
- Two to three years after being infected with COVID-19, participants scored on average significantly lower in cognitive tests (test of attention and memory) than expected. The average deficit was equivalent to 10 IQ points. Additionally, a substantial proportion reported severe symptoms of depression (about 1 in 5 people), anxiety (1 in 8), fatigue (1 in 4), and subjective memory problems (1 in 4), with these symptoms worsening over time.
- Although in many people these symptoms at two to three years were already present six months post-infection, some people also experienced new symptoms two to three years after their infection that they were not experiencing before. New symptoms often emerged in individuals who already exhibited other symptoms at six months post-infection. This suggests that early symptoms can be predictive of later, more severe issues, underscoring the importance of timely management.
- More than one in four participants reported changing their occupation and many gave poor health as a reason. Occupation change was strongly associated with cognitive deficits and not with depression or anxiety. This suggests that many people who changed occupation in the months and years after COVID-19 did so because they could no longer meet the cognitive demands of their job, rather than for lack of energy, interest, or confidence.
- The degree of recovery at six months post-COVID-19 is a strong predictor of longer-term psychiatric and cognitive outcomes. Intervening early to manage symptoms could prevent the development of more complex syndromes and improve overall recovery trajectories.
Dr. Maxime Taquet, NIHR Academic Clinical Lecturer in the Department of Psychiatry at Oxford, who led the study said, "These findings help us understand the burden of brain symptoms that people experience years after hospitalization for COVID-19, who is most at risk, and their impact on their ability to work. This is important for policymakers and clinicians, and to help target preventive interventions."
Professor Paul Harrison, Professor of Psychiatry at the University of Oxford, said, "Understanding the long-term cognitive and psychiatric consequences of COVID-19 hospitalization is important for many people, both patients and health professionals alike. We hope these findings will stimulate more research into the development of effective interventions to help prevent and treat these brain consequences of COVID-19."
Professor Chris Brightling, Clinical Professor of Respiratory Medicine at the University of Leicester, said, "This study reveals important long-term brain-related symptoms following COVID-19 and highlights the urgent need for better disease understanding of long-COVID, and new treatments."
The researchers caution that while this study provides insights into the long-term effects of COVID-19, further research is essential to develop effective interventions. Understanding the biological mechanisms driving these symptoms and identifying therapeutic strategies to promote cognitive recovery or prevent further decline are crucial next steps, they say.
The study sample was made up of individuals who were hospitalized during the first wave of the pandemic (and hence not vaccinated at the time of the infection) and who consented to follow-up assessments (only 20% of those invited), which may mean the findings are not generalizable to others (for example, people who did not require admission due to COVID-19).
PHOSP-COVID is a consortium of scientists from across the UK, researching long-term health outcomes for patients hospitalized with COVID-19.
More information: Maxime Taquet et al, Cognitive and psychiatric symptom trajectories 2–3 years after hospital admission for COVID-19: a longitudinal, prospective cohort study in the UK, The Lancet Psychiatry (2024). DOI: 10.1016/S2215-0366(24)00214-1




















