August 16, 2013 feature
Breath and butter: Resolving cholesterol's role in human lung surfactants
(Medical Xpress)—Pulmonary surfactants are phospholipoproteins (surface-active lipoprotein complexes) that reduces alveolar surface tension through an air-water hydrophilic/hydrophobic interface. Pulmonary, or lung, surfactants play several vital roles in lung function, including minimizing the energy needed to breathe, increasing pulmonary compliance (the ability of lungs to expand), preventing atelectasis (collapse of the lung at the end of expiration), reversing airway collapse, and regulating alveolar size. However, there are a number of diseases, such as neonatal respiratory distress syndrome (NRDS), congenital surfactant deficiency and pulmonary alveolar proteinosis, which require replacement pulmonary surfactants. In NRDS, for example, while replacement lung surfactants have dramatically reduced premature infant mortality, clinical lung surfactants vary widely in composition, requiring a deeper understanding of the function that each type of surfactant molecular performs. Recently, scientists working with lipid–cholesterol nanodomain complexes at University of California, Santa Barbara and University of Minnesota, Minneapolis demonstrated that small cholesterol fractions reduce surfactant interface viscosity by orders of magnitude while leaving compressibility and collapse unchanged. The researchers conclude that these results suggest the possibility of clinical control over surfactant spreadability.
Prof. Joseph A. Zasadzinski discussed the research he, KyuHan Kim and their colleagues performed with Medical Xpress. "One of the questions that puzzles me is that lung surfactant stays in the deep lung, even though there is a strong surface tension gradient of low surface tension in the deep lung – especially during exhalation – and a higher surface tension in the bronchi," Zasadzinski tells Medical Xpress. "This should pull surfactant towards the bronchi. Moreover, he points out, if the surfactant film is viscous, this will cause the surfactant to start to flow out of the lungs – and the lower the viscosity, the faster the flow. However, if the film is elastic, then there is a force preventing the surfactant from flowing out of the lungs, so not as much surfactant is lost.
"For a clinical surfactant," Zasadzinski continues, "the opposite scenario is true. A baby born without surfactant," he illustrates, "has a high surface tension in the lungs, which makes it impossible to expand the lungs against the forces of surface tension. Therefore, a good replacement surfactant has to spread quickly throughout the baby's lungs to lower surface tension – especially in the smallest alveoli – and it seems like it should therefore require a low viscosity material."
Another challenge the scientists faced was to understand the effects of small mole fractions of cholesterol. "Most surfactant research looks at 20 - 40 mol% cholesterol, as this is more common in cell membranes where the effects are large," says Zasadzinski. "However, for lung surfactants, we know that if we put more than about 15 mol%, the surfactant loses its ability to lower surface tension." In fact, he adds, this is one idea that could explain why getting blood and other cell debris in the lungs, as a result of accidents or disease, can cause acute respiratory distress syndrome, or ARDS: Cholesterol from the cells can mix with the lung surfactant and so the surfactant no longer functions properly. "ARDS is about 50% fatal," ARDS notes. "There is no generally accepted treatment, and our understanding is limited." Moreover, most of the clinical surfactants used for premature babies today are animal extracts from cow (Survanta), pig (Curosurf) and calf (Infasurf) lungs, which are obtained by washing out the lungs of the animals along with a variety of cell debris and blood. The surfactant is extracted with various solvents, and then reconstituted in saline.
"Prior to about 10 years ago," Zasadzinski continues, "all clinical lung surfactants were carefully scrubbed of cholesterol. Then Infasurf came along, and left about 5 wt% in, and it worked just as well – if not better – than the others. However, no one knew what a little cholesterol could do until we started measuring the mechanical properties of monolayers, and saw that a little cholesterol made a lot of difference in surface viscosity. This, in turn, tells us how fast surfactant will cover an interface – which is vital, since when the material is given to a newborn, the surfactant has to spread out and cover the entire surface area of the lung very quickly."
Anecdotally, Zasadzinski illustrates, doctors find that Infasurf, which has cholesterol and the lowest viscosity, seems to act more quickly than Survanta, which has the highest viscosity in rescuing babies from respiratory distress syndrome. "The difference between the three surfactants is minimal 10 to 30 minutes later, and some doctors think Survanta is better over the long term – but we don't yet know why. However, now that we know how to manipulate viscosity using small mole fractions of cholesterol without changing much of anything else, we can start doing experiments on adsorption, bulk flow, and other factors, to see how the cholesterol impacts physiological features that are important to short-term rescue and long-term survival."
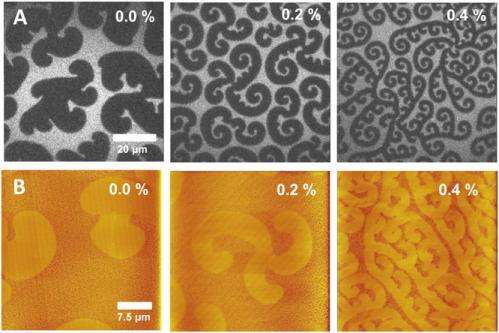
It has also been the case that controversy surrounds cholesterol's role in human lung surfactants, notes Zasadzinski. "Our pictures show that a small amount of cholesterol can break up lipids into smaller and smaller pieces that appear to be stable – the cellular membrane raft hypothesis." So-called lipid rafts are specialized membrane microdomains that compartmentalize cellular processes by serving as organizing centers for the assembly of signaling molecules, influencing membrane fluidity and membrane protein trafficking, and regulating neurotransmission and receptor trafficking. "Researchers have a good idea of a raft's utility in a cell membrane, but not of how to stabilize small areas of different compositions. Our system, which contains cholesterol, appears to be able to create very small compositional variations over very short length scales of 100 nm or less – so perhaps our system can tell us a bit more about the physics and chemistry that may lead to rafts."
Given the complex challenges the researchers faced, their key insights came from a single deceptively simple innovation. "My colleague Todd Squires and his graduate student – and later, my post-doc, Siyoung Choi – built a very sensitive monolayer rheometer that could not only measure the viscosities we found, but allowed us to simultaneously see what was going on using fluorescence microscopy," Zasadzinski explains. (A rheometer measures the way in which a liquid, suspension or slurry flows in response to applied forces.) "Seeing is believing! This one innovation helped us formulate our ideas and explanations." In addition, the researchers combined rheology (the physics of matter deformation and flow) with atomic force microscopy, and more recently, with X-ray diffraction, to start to relate surfactant rheology to monolayer morphology.
Experimentally, Zasadzinski points out that roughly 2 wt% cholesterol in 98 wt% Dipalmitoylphosphatidylcholine, or DPPC (a phospholipid that is the major constituent of pulmonary surfactant), decreased viscosity by a factor of more than 100. "This would be like taking a jar of honey and adding a spoonful of water and having the honey/water mix flow like water," he quips. "We also measured the lowest surface tension that we can get with these monolayers – and it turns out that cholesterol doesn't affect minimum surface tension until we get to ~10 mol%, and cholesterol doesn't change the surface area versus surface tension isotherms much at all, either. Only the viscosity changes – and it changes a lot."
Zasadzinski adds that they aren't sure why nothing other than the monolayer rheology changes with cholesterol. "We plan to use this new material to figure out what determines the minimum surface tension of a monolayer, which will help us design a better synthetic surfactant. Extracts vary in composition and often in efficacy from batch to batch, so figuring out what should go into a good surfactant is extremely important."
Moving forward, Zasadzinski says, their theory suggests that the viscosity should get very large once we get the monolayer close to collapse. "We're wondering if this large viscosity is what determines the minimum surface tension," he explains. "Our rheometer isn't capable of measuring such high viscosities, so we need to build a new one that can. We'll need stronger magnets and, probably, a bigger disc to float on the surface."
Zasadzinski mentions other areas of research that might benefit from their research. "We're also working on the effects of lipid organization in multiple sclerosis, or MS, in which the myelin sheath starts to unravel around the nerve axons, causing difficulty in nerve electrical conduction. We've found that the lipids in myelin change with MS in a way that changes the interactions between lipid bilayers, which might help explain why the myelin sheath unravels. We don't use rheology as much in this case," he concludes, "but rely instead on force measurement in Jacob Israelachvili's lab at UC Santa Barbara and conjunction with my work in fluorescence microscopy to determine monolayer organization."
More information: Effect of cholesterol nanodomains on monolayer morphology and dynamics, PNAS Published online before print July 30, 2013, doi:10.1073/pnas.1303304110
© 2013 Medical Xpress. All rights reserved.


















