3-D heart sock could replace pacemaker
(Medical Xpress)—An international research team that includes a University of Alberta engineering professor has designed a 3-D silicone "heart sock" that could eventually replace the venerable pacemaker.
Hyun-Joong Chung, professor of chemical and mechanical engineering at the University of Alberta, John Rogers, professor of engineering and chemistry at the University of Illinois, and Rogers' research group were co-authors of two recent articles published in Nature Communications and in Advanced Healthcare Materials on the development of the heart sleeve, which is designed to monitor vital signs.
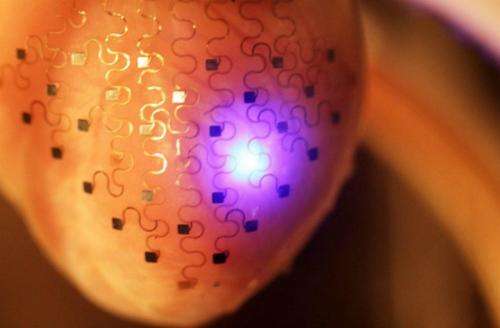
"My role specifically involved developing the first stretchable multiplexing chemical sensor, namely a pH sensor with multichannel mapping ability," said Chung. "The pH sensor array was embedded in the heart sock format, enabling real-time observation of the heart's chemical activities."
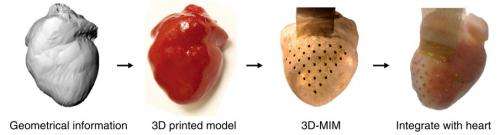
The researchers embedded 68 tiny sensors into a sheet of silicone that they fit around a 3-D printed replica of a rabbit heart. The circuits were laid out in a curved, S-shaped design that allows them to stretch and bend without breaking.
The heart sock physically resembles the shape of the pericardium, the naturally occurring membrane surrounding the heart. The sensors in the soft, flexible membrane track vital signs such as temperature, mechanical strain and pH. The device is designed to maintain a stable fit to the heart tissue, while exerting minimal force on the contracting and relaxing heart muscle.
The heart sock could be used to identify critical regions that indicate the origin of conditions such as arrhythmias, ischemia or heart failure—information that could guide therapeutic interventions.
The finished design will feature electrodes capable of regulating heartbeat, like a pacemaker, and it could counteract heart attacks. Although human trials may be a ways down the road, doctors and researchers recognize the significant potential of the technology.
The team is now looking at ways to dissolve the implant in the body once it is no longer needed and finding the optimal way to power the electrodes embedded in the device. They are also looking at opportunities to use the device to monitor other organs.
"I am currently pursuing various polymeric material systems that are stretchable and can be installed into living organs," Chung said. "One can simply envision cell scaffolds or surgical adhesives from such an approach."
Chung notes that many of the key technologies from this research could also be adapted to industrial uses, such as wear-resistant coatings for drills.
"The next step will be to develop a novel processing pathway to fabricate non-conventional electronic devices," he said.
More information: Lizhi Xu, et al. "3D multifunctional integumentary membranes for spatiotemporal cardiac measurements and stimulation across the entire epicardium." Nature Communications 5, Article number: 3329 DOI: 10.1038/ncomms4329.
Chung, H.-J., Sulkin, M. S., Kim, J.-S., Goudeseune, C., Chao, H.-Y., Song, J. W., Yang, S. Y., Hsu, Y.-Y., Ghaffari, R., Efimov, I. R. and Rogers, J. A. (2014), "Stretchable, Multiplexed pH Sensors With Demonstrations on Rabbit and Human Hearts Undergoing Ischemia." Advanced Healthcare Materials, 3: 59–68. doi: 10.1002/adhm.201300124



















