Study unlocks secret of common HIV strain
A discovery that the most common variant of the HIV virus is also the "wimpiest" will help doctors better treat millions of individuals around the world suffering from the deadly disease, according to one of the world's leading HIV/AIDS researchers. The findings were announced today in the journal EBioMedicine.
"HIV is one of the most diverse viruses that infect our human population," said Microbiology & Immunology professor Eric Arts, Canada Research Chair in HIV Pathogenesis and Viral Control. "We need to know how we are to treat these patients and how they respond to treatment when they are infected. That is one of the most difficult aspects for us to deal with in terms of developing a vaccine – the fact we have so many strains."
HIV – or human immunodeficiency virus – attacks and destroys infection-fighting cells of the immune system. Without treatment, HIV gradually destroys the immune system and advances to AIDS – or acquired immunodeficiency syndrome. AIDS is the most advanced stage of HIV infection.
According to the United Nations, there were approximately 36.7 million people worldwide living with HIV/AIDS at the end of 2015. Of these, 1.8 million were children under 15 years old. An estimated 2.1 million individuals worldwide became newly infected with HIV in 2015; that number includes 150,000 children who mostly live in sub-Saharan Africa who were infected by their HIV-positive mothers during pregnancy, childbirth or breastfeeding.
The majority of those living with the virus are infected with HIV strains not found in North America or Europe, Arts explained, and, as a consequence, researchers know less about them.
In a research project he began almost 15 years ago while at Case Western Reserve University, Arts explored how the various strains of the HIV virus advance in the body. He sought out differences in the strains and how those differences might impact treatment.
HIV is a complex and diverse disease, Arts stressed.
"We don't have one virus infecting 33 million people; we have 33 million people infected with 33 million types of viruses," he said. "We can't look at it as a single strain anymore. We need to look at the differences that exist."
HIV Type 1 (HIV-1) and HIV Type 2 (HIV-2) are two distinct viruses. Generally, when people speak about HIV, they are referring to HIV-1. HIV-2 is relatively uncommon outside of West Africa. Strains of HIV-1 are classified into four groups – Group M, N, O and P. Of those, Group M – or 'Major' – is responsible for the majority of global HIV cases.
Within Group M, there are nine genetically distinct subtypes – A, B, C, D, F, G, H, J and K. The dominant subtype in the Americas, Western Europe and Australasia is Subtype B. As a result, the majority of HIV clinical research has been conducted in these populations despite the fact they represent only one in 10 global HIV infections.
In contrast, less research is available for Subtype C, although just under half of all people living with HIV have that subtype. The subtype is common in the countries of southern Africa, as well as in the horn of Africa and India.
In screening approximately 300 women in Zimbabwe, Thailand and Uganda newly infected with HIV starting in the early 2000s, Arts and his team studied the length of time it took the disease to go from HIV infection to AIDS. He found Subtype C replicated poorly and slowly in patients – earning it the 'wimpy' moniker among its fellow subtypes.
"This study was a once-in-a-lifetime opportunity for the world to see how patients progress to AIDS and the reasons why. We could analyze the disease progression until they reached AIDS, which is when we started treatment," said Arts, noting this progression took anywhere from five to nine years.
Currently, such a study would be considered unethical, he added, as treatment now starts much earlier for HIV-infected patients. His team was among the first to bring treatment for AIDS patients, in advance of any global treatment programs arriving in Africa.
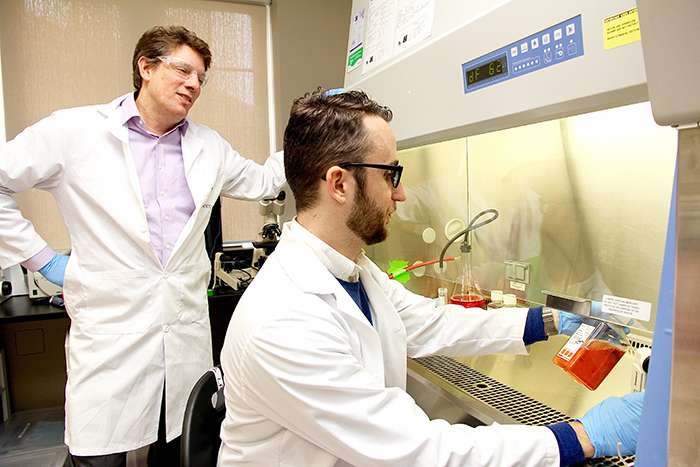
Graduate student Colin Venner, who assisted Arts with the research, said they would put Subtype C into "boxing matches" in a controlled lab environment to test its strength against other subtypes.
"We don't really have a way to directly visualize what's going on. But once we pull it out, we can see who wins and, in fact, Subtype C is 'wimpy' because it will always be competed to non-existence," Venner said. "We won't be able to find Subtype C at all in these cultures in many cases. It is 100-to-1,000-fold less able to replicate than some other subtype strains."
Subtype C has exploded since the early 1990s, added Venner, drawing many to conclude it would be the strongest virus subtype. However, the HIV virus is usually transmitted during the period patients show no symptoms and are thereby unaware of their condition. A slowly revealing subtype, like Subtype C, might be more likely to be spread given a longer period of no symptoms.
"The longer a patient is asymptomatic, the more likely they may be to transmit it is one of the thoughts that we're working on right now," Venner said.
With Subtype C being the dominant strain in the HIV population, Arts' findings may soon have an impact on potential treatments for HIV patients.
"Knowing the differences in virulence (the capability of a microorganism to cause disease) of these different subtypes has an impact on how we treat with drugs and how we administer vaccines throughout the world," said Arts, adding, unfortunately, there is still no vaccine effective in protecting against HIV. "But, in treatment, if we know a patient progresses very slow to disease and the virus is having a minimal impact on the immune system, all the devastating consequences of delaying treatment, as we saw in North America, may not be as pronounced in patients infected with Subtype C."
These potential treatments, however, don't come without some ethical debate.
"When we're looking at billions and billions of dollars a year to treat the global epidemic, we might have to look at it as to who needs treatment immediately and who can be delayed," Arts said. "That's very controversial but it is something we have to consider."
More information: Infecting HIV-1 Subtype Predicts Disease Progression in Women of Sub-Saharan Africa. DOI: dx.doi.org/10.1016/j.ebiom.2016.10.014
















