Research yields new insights into the cause of diabetes
The cause of insulin-dependent, permanent, diabetes in newborn babies may be a deficiency in the enzyme Pancreatic Endoplasmic Reticulum Kinase (PERK) during a critical period of development before birth, according to a new hypothesis put forward by a team of researchers from Penn State University.
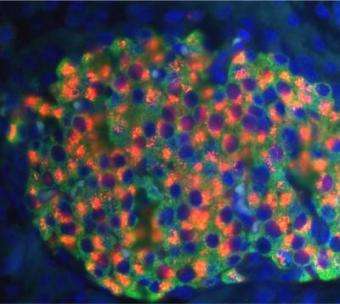
In this most severe type of diabetes, individuals are unable to regulate glucose normally because they have few insulin-producing beta cells in their pancreas and the remaining cells do not produce enough insulin. Using special strains of mice bred to be PERK-deficient, the researchers demonstrated that the lack of this enzyme blocked the proliferation of beta cells, hampered the normal functioning of beta cells, and also kept beta cells from clustering into islets.
"What happens during fetal development predisposes people either to be able to maintain glucose levels normally or to have diabetes," says team leader Douglas Cavener, professor and head of the Department of Biology. The research results will be published in the journal Cell Metabolism on 6 December 2006.
The team, consisting of graduate students Wei Zhang, Yulin Li and Kaori Iida, Postdoctoral Fellow Daorong Feng, and Research Assistant Professor Barbara McGrath, made use of the lab's earlier discovery that mice deficient in PERK show many parallels to human sufferers of Walcott-Rallison Syndrome (WRS), in which diabetes is combined with skeletal and growth abnormalities. The research provided an experimental model for investigating the cause of permanent neonatal diabetes that was more revealing than cell culture studies.
"Being able to develop special strains of mice that are PERK-deficient in specific organs or tissues was vital to our research," says Cavener. "These mice allowed us to discover exactly how PERK participates in the development and growth of the beta cells in the pancreas that secrete insulin. Using genetics in this way lets the organism tell you what is important to normal function."
Normally, the beta cells of the pancreas respond to high levels of glucose in the blood by producing the precursor of insulin -- proinsulin -- in the endoplasmic reticulum. Inside this and other organelles, the proinsulin is assembled and modified into insulin. Then the hormone is exported from the cell to stimulate other tissues to take up glucose and generate energy.
PERK-deficient mice differ significantly from normal mice. At birth, PERK-deficient mice have only about one-half the mass of beta cells that normal mice have. During the first few weeks after birth, PERK-deficient mice have fewer and fewer beta cells compared to normal mice and the remaining cells do not function normally in producing insulin. By three weeks after birth, the PERK-deficient mice are fully diabetic and have only one-tenth the mass of beta cells as normal mice.
Until now, the dominant hypothesis of the cause of diabetes in mice and humans deficient in PERK was developed by Heather Harding and David Ron, of New York University Medical Center, in 2001. They suggested that too much proinsulin in the endoplasmic reticulum triggers a stress response and causes many beta cells to die. The shortage of beta cells in PERK-deficient mice was thought to be caused by a high death rate of those cells.
Data collected by the Cavener team casts doubt on this hypothesis. First, they found that mice deficient in PERK made new beta cells at a much lower rate than normal mice. The mass of beta cells in deficient mice only doubled during the first few weeks of life, while that in normal mice increased twenty-fold. Second, the Penn State group found the rate of beta-cell death in PERK-deficient mice was not significantly different from that in normal mice. Finally, the team did not detect molecular markers of endoplasmic reticulum stress in the beta cells of their PERK-deficient mice.
The alternative hypothesis of the Penn State Team is that PERK deficiency blocks both the proliferation of beta cells after birth and the differentiation of those cells into fully functioning units. They found that thirty to forty percent of the beta cells of PERK-deficient mice are physically unusual. The most obvious abnormality is that proinsulin is found the endoplasmic reticulum, instead of being found in or around the nucleus. Apparently, proinsulin is produced as usual, but the normal modification process is blocked, leaving large quantities of proinsulin trapped inside the enlarged and distended organelle.
Another important finding was that beta cells in these mice do not develop into organized clusters or islets within the pancreas. Normally, the protein GLUT2 transports glucose across plasma membranes among the islets, triggering the secretion of insulin in the beta cells. But without the islet architecture, communication among the beta cells breaks down and the cells fail to respond to glucose by secreting insulin. Thus, PERK-deficiency both hampers cell-to-cell signaling of glucose levels and greatly diminishes insulin production at the cellular level.
The Penn State team's understanding of the role of PERK was advanced by additional experiments to pinpoint the time during development when PERK is required. Cavener's team found that PERK must be expressed during a critical period between 13.5 fetal days and 4 days after birth if the beta cells of the pancreas are to regulate glucose normally for the rest of the animal's life. PERK may play an essential role in sensing fetal environment and modulating the development of beta cells in response to it.
"The genetic program of the fetus and the in-utero environment work together to set up the apparatus that regulates glucose in postnatal life," Cavener explains.
Source: Penn State




















