In response to chemo, healthy cells shield cancer cells
Many times, cancer patients respond very well to chemotherapy initially only to have their disease return, sometimes years later. Now researchers reporting in the October 29th issue of the journal Cell, a Cell Press publication, have new insight into the factors that allow some lingering tumor cells to resist treatment and to seed that kind of resurgence.
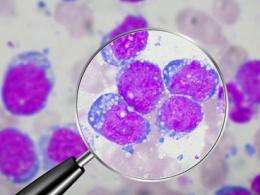
Contrary to expectations, it appears that the answer doesn't necessarily lie in the cancerous cells themselves. The evidence based on studies of mice with lymphoma shows that cues coming from healthy cells in response to the stress of chemotherapy can protect their cancerous neighbors, allowing them to persist in select refuge sites.
"It's a surprising finding, but it's consistent with organ homeostasis," said Michael Hemann of Massachusetts Institute of Technology. For an organ to maintain itself, it has to respond to stressful conditions, he explained. "In this case, the stress response is to chemo. The chemotherapy kills tumor cells while it elicits stress responses that protect a subset of tumor cells in select locations from drug action."
That stress signal, a molecule called IL-6, allows cancer cells to persist in the thymus. They have evidence that those surviving cells are relevant to disease progression, as removal of thymus tissue prolonged the animals' tumor-free survival.
The researchers further showed that human liver cancer cells release IL-6 as well when treated with the chemotherapeutic agent doxorubicin. When they combined chemotherapy with a treatment that blocks IL-6 signaling, cancer cells were more likely to die.
If the findings in mice and human cells prove relevant in human cancer, they suggest that treatments designed to work against IL-6 might be combined with chemotherapy to reduce the chance that a cancer will recur. "The approach to cancer is usually single agents," Hemann said. "Our data suggest that a combination of DNA damaging chemotherapy or radiation plus treatments designed to block pro-survival pathways would be the most potent therapy."
Anti-IL-6 treatments are already in development for patients with arthritis, Hemann said, as IL-6 is perhaps best known for its role in inflammation.
The results come at an important time. "While significant progress has been made in the application of chemotherapy in the past 40 years, most chemotherapeutic regimens ultimately fail to cure patients," the researchers wrote. "Even tumors that show dramatic initial responses to therapy frequently relapse as chemoresistant malignancies."
In the past, most studies of resistance to chemotherapy had focused on changes within the cancer cells themselves. The cells were thought to pump drugs out faster, to activate enzymes that detoxify the chemotherapeutic agent or to lose the activity of genes involved in cell death.
But recent data began to suggest that there was another way; that resistance to chemo could arise from external factors, such as immune signaling molecules (cytokines) or growth factors. The new study adds to that evidence and is one of very few to consider the role of the tumor microenvironment in chemotherapeutic outcome, the researchers say. In other words, it's all about location.
We show that resistance to chemotherapy "relates to where the tumor is. There are some locations that are inherently protective," Hemann said.
He said he expects this survival mechanism may play a role in other forms of cancer. He notes that IL-6 is present in many microenvironments in the body. Earlier studies have also shown blood levels of IL-6 to rise in those with many types of cancer. Those high IL-6 levels have also been linked to poor survival and accelerated disease progression in a variety of cancers, including lymphomas.
Hemann said the findings show how important basic biology can be to developing new and better combination therapies to fight cancer. His team plans to conduct pre-clinical studies to see whether chemotherapy plus anti-IL-6 therapies can improve outcomes in animals with lymphoma and hepatocellular carcinoma.













