Rebooting the system: Immune cells repair damaged lung tissues after flu infection
There's more than one way to mop up after a flu infection. Now, researchers from the Perelman School of Medicine at the University of Pennsylvania report in Nature Immunology that a previously unrecognized population of lung immune cells orchestrate the body's repair response following flu infection.
In addition to the looming threat of a deadly global pandemic, an estimated 200,000 people are hospitalized because of the flu and 36,000 die each year in the US, according to the Centers for Disease Control. However, many influenza-related deaths are not a direct result of the invading virus but instead are linked to the body's failure to effectively repair and restore lung tissues after it has been damaged by the virus. However, the processes that promote lung tissue repair have remained elusive.
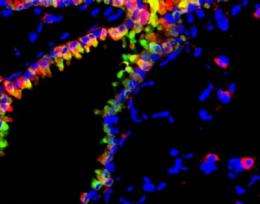
In this new report, David Artis, PhD, associate professor of Microbiology; Laurel Monticelli, a PhD student in the Artis lab; and colleagues observed that flu-infected mice without a population of immune cells called innate lymphoid cells suffered poor lung function leading to eventual death. The team also found that those innate lymphoid cells produced a growth factor called amphiregulin. Infusion of innate lymphoid cells or amphiregulin to the lungs of infected mice normalized lung function, suggesting that the activation of these cells is central to tissue repair at lung surfaces.
Notably, the researchers found that innate lymphoid cells don't attack the virus per se, as other immune cells do; rather, they spur the proliferation of cells that line the lung, which aids in wound healing of the lung tissues that have been severely damaged as a result of the viral infection.
Based on these findings, this lung cell population could also promote wound healing following other respiratory infections and possibly drive tissue remodeling in situations of non-infectious lung injury and inflammation such as asthma, explains first author Monticelli.
In order to extend these studies to human health, Artis and his team collaborated with researchers at Columbia University to identify a population of innate lymphoid cells that is resident in healthy human lung tissue similar to the cells found in mice. These findings raise the possibility that these cells may also orchestrate lung tissue repair in humans and that targeting activation of innate lymphoid cells through amphiregulin or other proteins may speed tissue recovery in patients suffering from respiratory illnesses.
"The identification of innate lymphoid cells in the lung, and new studies from multiple research groups illuminating their previously unrecognized functions in diverse disease processes could help in the design of new drugs to prevent or better fight many common infectious or inflammatory diseases," concludes Artis.
















