Scientists aim to kill lung tumors
Lung cancer is the leading cause of cancer death throughout the world. Standard treatment methods do not usually result in long-term recovery. In addition to the proliferation of the tumour cells, the growth of blood vessels controls tumors development. The blood vessel growth is controlled by several signalling molecules.
Scientists from the Max Planck Institute for Heart and Lung Research in Bad Nauheim and Justus Liebig University Giessen have discovered a molecule that plays a key role in this process. They succeeded in reducing tumour growth in their experiments by blocking the phosphodiesterase PDE4.
Lung cancer mainly affects smokers; however the disease can also be caused by contact with carcinogenic substances like asbestos. Chemotherapy or radiotherapy often prove insufficient in treating the disease. Hence, scientists are engaged in an intensive search for ways of halting the growth of lung tumours. The blood vessels that supply the tumour with nutrients offer a potential point of attack.
New blood vessels form to ensure an adequate supply of nutrients to the growing tumour. The growing tissue is immediately penetrated by blood vessels. The growth of the blood vessels is regulated by the tumour cells using a complex signal cascade, which is triggered initially by a low oxygen content (hypoxia) in the tumour tissue. "This state, which is known as hypoxia prompts the activation of around 100 genes in the tumour cells," explains Rajkumar Savai, research group leader at the Max Planck institute. "In addition to the growth of blood vessels, hypoxia also stimulates the proliferation of lung cancer cells." Three molecules play a particularly important role in this process. The activation of the genes at the beginning of the cascade is triggered by the transcription factor HIF and a messenger molecule, cAMP, is involved again at the end of the cascade. The researchers examined the third molecule that acts as a link between these two molecules in detail.
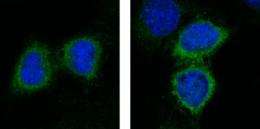
The molecule in question is a phosphodiesterase, PDE4. The scientists from Bad Nauheim and Giessen were able to demonstrate in their study that various sections of PDE4 have binding sites for HIF.
The researchers then tested the influence of a PDE4 blockade on the cells from ten different cell lines, which are characteristic of around 80 percent of lung cancers, in the laboratory. The rate of cell division in the cells treated with a PDE4 inhibitor was significantly lower and the HIF level also declined as a result.
The effect in the tumour bearing mice was particularly obvious. To observe this, the Max Planck researchers implanted a human tumour cell line under the skin of nude mice and treated the animals with the phosphodiesterase 4 inhibitor.
Tumour growth in these animals declined by around 50 percent. "Our microscopic analysis revealed that the blood vessel growth in the tumours of the mice that had been treated with the inhibitor was significantly reduced. We also observed indicators of decelerated cell division in the tumour cells. Overall, the tumour growth was strongly curbed."
Werner Seeger, Director of the MPI and Medical Director of the JLU University Hospital Giessen, reports: "We were able to show that PDE4 plays an important regulation function in cell division in lung tumours and in the development of blood vessels in cancer. Therefore, we hope that we have found a starting point for the development of a treatment here." In the view of tumour specialist Friedrich Grimminger, Chairman of the Department of Medical Oncology in Giessen, it may be possible in future to combine the inhibition of PDE4 with traditional radiotherapy or chemotherapy. In this way, the effect of the traditional treatment measures could be reinforced and patient prognoses may improve as a result. However, further laboratory studies are required before clinical tests can be carried out.
More information: Oncogene (2012). doi:10.1038/onc.2012.136















