Superbug MRSA identified in US wastewater treatment plants
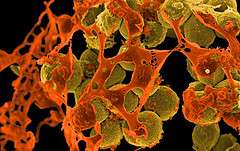
A team led by researchers at the University of Maryland School of Public Health has found that the "superbug" methicillin-resistant Staphylococcus aureus (MRSA) is prevalent at several U.S. wastewater treatment plants (WWTPs). MRSA is well known for causing difficult-to-treat and potentially fatal bacterial infections in hospital patients, but since the late 1990s it has also been infecting otherwise healthy people in community settings.
"MRSA infections acquired outside of hospital settings – known as community-acquired MRSA or CA-MRSA– are on the rise and can be just as severe as hospital-acquired MRSA. However, we still do not fully understand the potential environmental sources of MRSA or how people in the community come in contact with this microorganism," says Amy R. Sapkota, assistant professor in the Maryland Institute for Applied Environmental Health and research study leader. "This was the first study to investigate U.S. wastewater as a potential environmental reservoir of MRSA."
Because infected people can shed MRSA from their noses and skin and through their feces, wastewater treatment plants are a likely reservoir for the bacteria. Swedish researchers have previously identified the presence of MRSA in WWTPs in Sweden, and this new UMD-led study confirms the presence of MRSA in U.S. facilities. The study was published in the November issue of the journal Environmental Health Perspectives.
The research team, including University of Maryland School of Public Health and University of Nebraska Medical Center researchers, collected wastewater samples throughout the treatment process at two Mid-Atlantic and two Midwestern WWTPs. These plants were chosen, in part, because treated effluent discharged from these plants is reused as "reclaimed wastewater" in spray irrigation activities. The researchers were interested in whether MRSA remained in the effluent.
They found that MRSA, as well as a related pathogen, methicillin-susceptible Staphylococcus aureus (MSSA), were present at all four WWTPs, with MRSA in half of all samples and MSSA in 55 percent. MRSA was present in 83 percent of the influent– the raw sewage – at all plants, but the percentage of MRSA- and MSSA-positive samples decreased as treatment progressed. Only one WWTP had the bacteria in the treated water leaving the plant, and this was at a plant that does not regularly use chlorination, a tertiary step in wastewater treatment.
Ninety-three percent of the MRSA strains that were isolated from the wastewater and 29 percent of MSSA strains were resistant to two or more classes of antibiotics, including several that the U.S. Food and Drug Administration has specifically approved for treating MRSA infections. At two WWTPs, MRSA strains showed resistance to more antibiotics and greater prevalence of a gene associated with virulence at subsequent treatment stages, until tertiary chlorination treatment appeared to eliminate all MRSA. This suggests that while WWTPs effectively reduce MRSA and MSSA from influent to effluent, they may select for increased antibiotic resistance and virulence, particularly at those facilities that do not employ tertiary treatment (via chlorination).
"Our findings raise potential public health concerns for wastewater treatment plant workers and individuals exposed to reclaimed wastewater," says Rachel Rosenberg Goldstein, environmental health doctoral student in the School of Public Health and the study's first author. "Because of increasing use of reclaimed wastewater, further research is needed to evaluate the risk of exposure to antibiotic-resistant bacteria in treated wastewater."
More information: The paper Methicillin-Resistant Staphylococcus aureus (MRSA) Detected at Four U.S. Wastewater Treatment Plants was written by Rachel E. Rosenberg Goldstein, Shirley A. Micallef, Shawn G. Gibbs, Johnnie A. Davis,Xin He, Ashish George, Lara M. Kleinfelter,Nicole A. Schreiber, Sampa Mukherjee, Amir Sapkota,Sam W. Joseph, and Amy R. Sapkota and published in the November 2012 issue of Environmental Health Perspectives. ehp.niehs.nih.gov/2012/11/1205436/















