A stop sign for cancer
A particularly aggressive form of leukemia is the acute lymphoblastic leukemia (ALL). It is especially common among children and very difficult to treat. Researchers from the University of Veterinary Medicine, Vienna have now discovered completely new targets for the treatment of blood cancers. Studying the cancer protein STAT5, the scientists found new opportunities for the development of effective anti-cancer drugs. The research team published the scientific work, which could also become relevant for other types of cancer, in the journal Leukemia.
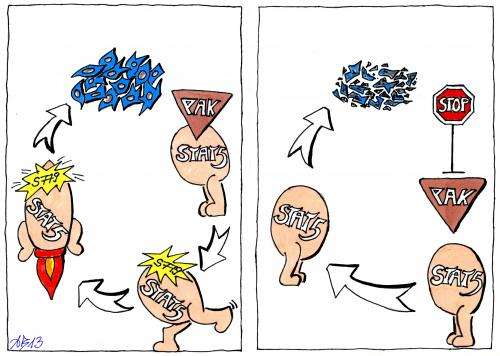
Proteins in cells communicate like relay runners in a competition. The sticks that are transferred between the runners are the "signals". These signals are passed within the cell from one protein to another and ensure cell growth and survival. In cancer cells it is interesting approach to block this information cascade and thereby block the proliferation of cancer cells.
Essential for the signalling in cancer cells is the protein STAT5. It is known that STAT5 is overstimulated in many cancers. It forwards signals in an uncontrolled manner and is ultimately responsible for the excessive cell division of cancer cells. In mice that suffer from leukemia, it has already been shown, that the elimination of STAT5 makes the animals gain health again. Therefore, the importance of the protein in cancer is obvious. The researchers now want to apply this information on cancer therapy in humans.
Slowing down STAT5
The research team led by Veronika Sexl from the Institute of Pharmacology and Toxicology at the Vetmeduni Vienna took a closer look at STAT5. Using leukemia as a model disease, the team looked for therapeutically exploitable attack points on the protein and they actually identified such. The shutdown of two distinct signals of STAT5 led to a significantly later progression of leukemia in mice compared to animals that harboured the unmodified STAT5. One of these two therapeutically relevant sites is of particular importance: "The shutdown of the site Serin779 on STAT5 makes it impossible for STAT5 to fulfil its role as a relay runner and migrate into the nucleus. Thus, the effect of STAT5 is inhibited", says Hölbl-Kovacic, one of the lead authors of the pioneering publication.
Interrupting the relay race at several points
In a large-scale screening, the co-lead author Angelika Berger identified those relay runners that act before Serin779, the so-called PAK (p21 activated kinase). This means that PAK has control over STAT5 and activates it. By inhibiting PAK, STAT5 is turned off and disconnected from the relay race. The cancer researchers also found that PAK is still active, when cancer cells have already been treated with the current standard therapeutic agent Imatinib. This means that a potential new drug that acts on PAK could be well used in combination with Imatinib. Such a strategy would be of great importance in patients that no longer respond to Imatinib and are "therapy-resistant". PAK kinases thus represent a new therapeutic target, which is independent of previous treatment methods.
STAT5 has a role in many cancers
Angelika Berger explains: "So far, the PAK kinases have received relatively little attention in cancer therapy. However, they could be beneficial for a wide range of applications. All types of cancers, in which STAT5 plays a role, could be treated by this system in a new way. Those are the leukemias but also a number of other diseases such as breast cancer or prostate cancer."
More information: "PAK-dependent STAT5 serine phosphorylation is required for BCR-ABL-induced leukemogenesis." A Berger, A Hoelbl-Kovacic, J Bourgeais, et al. Leukemia. Advance online publication 13 December 2013. DOI: 10.1038/leu.2013.351












