How does H. influenzae thrive in COPD patients?
It can be almost painful to watch individuals with chronic obstructive pulmonary disease (COPD) breathe. When they're not coughing, they're fighting for every breath. Approximately 24 million Americans struggle with COPD—which typically worsens over time and is the third most common cause of death.
A lung infection can be a life-threatening event for someone with COPD.
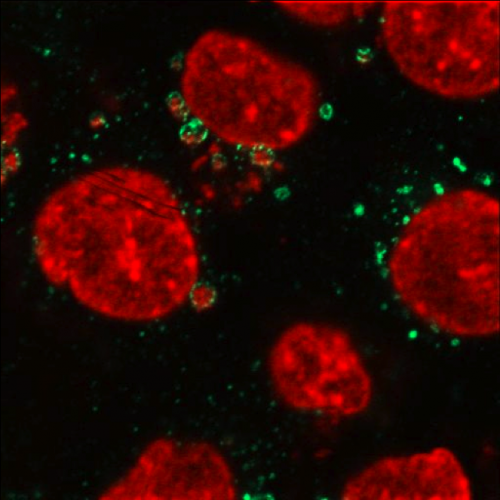
Researchers now say that the bacterium, non-typeable Haemophilus influenzae (NTHI), may be a key factor in the hallmark signs of COPD: airway inflammation and impaired pulmonary function. While NTHI frequently exists in healthy humans without causing any problems, it seems to proliferate and flourish in the lower respiratory airways of patients with COPD.
The University at Buffalo has recently been awarded a $2,287,587 five-year National Institutes of Health grant to study and detail the mechanisms that allow NTHI to infect and survive in the airways of adults with COPD. This understanding may lead to new drugs that can effectively reduce NTHI infections and save lives.
This study represents the 28th year of a long running grant to study NTHI.
"In healthy people, H. influenzae is present in the throat but not in the lower airways of the respiratory tract," said Timothy Murphy, MD, SUNY Distinguished Professor and UB senior associate dean for clinical and translational research in the UB School of Medicine and Biomedical Sciences and the principal investigator on the grant.
"People with COPD, however, have diseased airways which impairs the normal protective responses. Thus H. influenzae is present in the lower airways of people with COPD. It is also the most important bacterial cause of exacerbations or the worsening of COPD symptoms, and can lead to serious complications."
The three aims of the grant are to study how NTHI is able to persist from months to years in airways; to assess potential vaccine antigens that are under development; and to assess how NTHI can survive repeated courses of antibiotic therapy.
The grant was first funded shortly after Murphy joined the UB medical school. Every three to five years, the grant was renewed by what's called a competitive renewal where scientists write a new grant that is reviewed and then competes with all other NIH grant applications.
Sanjay Sethi, MD, professor of medicine and chief of the Division of Pulmonary, Critical Care and Sleep Medicine, a co-investigator on the study, also collaborated with Murphy on the long-running study of adults with COPD.
The perfect score—a rare accomplishment – Murphy says was most likely related to several factors:
- An 18 year prospective study with this level of rigorously characterized bacterial strains is unique. No other set of strains collected longitudinally and with this level of detailed clinical data tied to each strain exists in the world.
- The application of state-of-the-art "next gen sequencing" to this unique set of strains is compelling. Sequencing technology is advancing so quickly that proposing such a large amount of sequencing just a few years ago would simply not have been feasible. Now this amount of sequencing can be performed readily.
- The specific questions that have been proposed to study in the grant's three aims will advance the field significantly.
- Determining genome sequences on this large unique set of well-characterized strains is likely to yield new and unexpected results. This is the "exploratory" nature of this grant.
In the study, how NTHI survives an onslaught of antibiotics will be handled by using an innovative Hollow Fiber Infection Model developed by Brian Tsuji, PharmD, UB associate professor of pharmacy practice and co-investigator on the grant.
Tsuji's model will expose NTHI to levels of antibiotics at the exact levels that occurred in COPD patients. Murphy says they will integrate these results with the results of genome analysis for a better understanding of antibiotic resistance and tolerance.
Michael Buck, PhD, assistant professor of biochemistry who oversees the UB Next Gen Sequencing Core is also working as a co-investigator and will be responsible for the genome sequencing
Murphy adds that the technicians who work in his lab are essential to making all of this work possible. They are Charmaine Kirkham, Aimee Brauer and Antoinette Johnson.
In the last 50 years, says Murphy, other than the development of antibiotics, there has been little progress in developing new treatments and prevention of infections in COPD.
"I am trying to understand the mechanisms by which H. influenzae causes infection so that these observations can be used to develop better treatments. This is an excellent example of translational research."














