Personalising treatment in idiopathic pulmonary fibrosis
Researchers in UCD Conway Institute have identified a potential biomarker of rapidly progressive pulmonary fibrosis and pinpointed a defective molecular function as a potential therapeutic target.
Planning treatment for patients with idiopathic pulmonary fibrosis (IPF) is difficult due to the unpredictable course the disease can take. Almost 15% of IPF patients die within 12 months of the initial diagnosis.
However, researchers led by Conway Fellow, Professor Seamas Donnelly of UCD School of Medicine & Medical Science and the Education & Research Centre, St Vincent's University Hospital have identified a potential biomarker of rapidly progressive disease and pinpointed a defective molecular function as a potential therapeutic target.
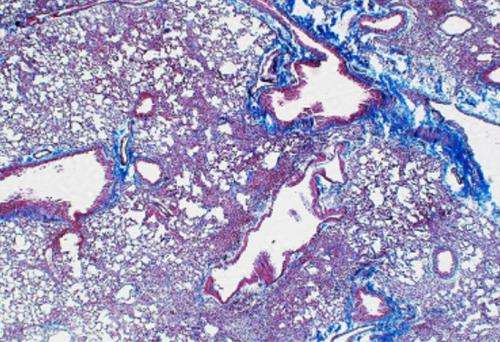
Idiopathic pulmonary fibrosis (IPF) is a fatal progressive interstitial pneumonia. This chronic inflammatory disease leads to the breakdown of normal lung architecture and the loss of lung function as a result.
In humans, the innate immune system is responsible for recognising tissue injury and infection. Toll-like receptor 3 (TLR3) is an innate immune system receptor involved in this process of identifying pathogens and defending against them.
Professor Donnelly and his team investigated whether a particular genetic defect in the TLR3 gene might disrupt the normal inflammatory response in IPF and accelerate the progression of the disease.
This specific genetic variation in one of component DNA building blocks of the TLR3 gene is named L412F single-nucleotide polymorphism (SNP).
The UCD research team in collaboration with colleagues in Ireland, the UK and in the USA examined the impact of defective TLR3 function in the lung and on the progression of IPF using lung fibroblasts from patients with and without TLR3 L412F single-nucleotide polymorphism (SNP) and in a laboratory model of the disease.
Commenting on the results, Dr Gordon Cooke, senior postdoctoral research fellow and one of the authors of the recently published article said, "This study identifies the TLR3 L412F polymorphism as a potential marker of rapidly progressive disease and defective TLR3 function represents a potential therapeutic target in IPF."
Professor Seamas Donnelly said, "Our findings suggest a strong mechanistic link between this candidate polymorphism and altered fibrosis, the immune response, and survival in patients. This opens the possibility of focused therapies aimed at restoring TLR3 function as well as supporting an approach to personalising therapy in IPF by identifying at an early stage those patients at significant risk and tailoring their treatment accordingly."
Patient cohorts from around the world were used to validate the study including those from St. Vincent's University Hospital, Dublin. Genotyping of patients was carried out in the UCD Conway genomics core facility. The research is supported by funding from the Health Research Board of Ireland, Science Foundation Ireland and the Irish Lung Foundation.
More information: Dwyer DN, Armstrong ME, Cooke G, Keane MP, Donnelly SC, et al. The Toll-like Receptor 3 L412F Polymorphism and Disease Progression in Idiopathic Pulmonary Fibrosis. American Journal of Respiratory & Critical Care Medicine. 188; 12, 1442-1450. December 15, 2013.













