New cancer vaccine approach directly targets dendritic cells
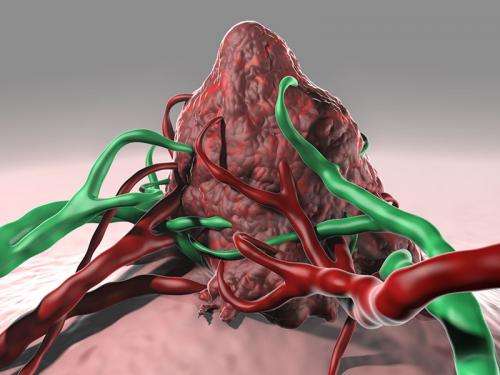
Celldex Therapeutics announced today that final data from its Phase 1 study of CDX-1401 in solid tumors, including long-term patient follow-up, have been published in Science Translational Medicine. The data demonstrate robust antibody and T cell responses and evidence of clinical benefit in patients with very advanced cancers and suggest that CDX-1401 may predispose patients to better outcomes on subsequent therapy with checkpoint inhibitors. CDX-1401 is an off-the-shelf vaccine consisting of a fully human monoclonal antibody with specificity for the dendritic cell receptor DEC-205 linked to the NY-ESO-1 tumor antigen. The vaccine is designed to activate the patient's immune system against cancers that express the tumor marker NY-ESO-1. While the function of NY-ESO-1 continues to be explored, references in the literature suggest that its expression might reflect the acquisition of properties that cancers find useful, such as immortality, self-renewal, migratory ability and the capacity to invade.
The Phase 1 study of CDX-1401 is the first clinical study to demonstrate that an off-the-shelf vaccine that targets dendritic cells in vivo through DEC-205 can safely lead to robust humoral and cellular immunity—overcoming a significant challenge in the development of protein based vaccines. Targeting protein antigens to the DEC-205 receptor on dendritic cells was pioneered by the late Ralph Steinman, MD, a member of Celldex's Scientific Advisory Board. Dr. Steinman received the 2011 Nobel Prize in Physiology or Medicine for his discovery of the dendritic cell and its role in adaptive immunity. This now-proven ability to target proteins, like NY-ESO-1, to dendritic cells to generate potent immune responses specific to these proteins represents a promising approach for the next generation of vaccines against pathogens and cancer.
"CDX-1401 offers a novel, well-tolerated and practical approach to generating protein specific immunity that can be readily combined with other treatment strategies to boost immunity against pathogens and tumors," said Dr. Madhav Dhodapkar, MBBS, Arthur H. and Isabel Bunker Professor of Medicine and Immunobiology, Chief of the Section of Hematology at the Department of Internal Medicine and Clinical Research Program Leader of the Hematology Program at Yale Cancer Center and lead author of the paper. "The preliminary findings in patients who received therapy with a checkpoint inhibitor following the vaccine provide further rationale for combination immunotherapy strategies, meriting further investigation."
Thomas Davis, MD, Senior Vice President and Chief Medical Officer of Celldex Therapeutics added, "CDX-1401 has overcome a significant historical challenge in the development of protein based vaccines by successfully targeting dendritic cells in vivo. It now sits at the forefront of a new generation of off-the-shelf dendritic cell targeted vaccines that we believe hold significant promise. Based on the results observed in this Phase 1 study, we expect CDX-1401 to enter at least two combination studies this year with both our own investigational therapies and external therapies in melanoma and other indications where we believe a dendritic cell vaccine regimen could play an important role." Initial results from the Phase 1 study of CDX-1401 were presented at the 2012 Society for Immunotherapy Annual Meeting. The manuscript published today expands upon this data and includes longer-term patient follow up.
CDX-1401 Phase 1 Study Overview and Results
The study was designed to assess the safety, immunogenicity and clinical activity of escalating doses of CDX-1401 with TLR agonists (resiquimod and/or Poly ICLC (HiltonolTM) in 45 patients with advanced malignancies refractory to all available therapies. CDX-1401 was well tolerated, with no dose limiting or grade 3 toxicities reported. The most frequently reported adverse events were administration site reaction, fatigue, nausea and chills. Treatment induced humoral and cellular immunity to NY-ESO-1 in patients with NY-ESO-1 expressing tumors across various dose levels and adjuvant combinations.
Significant anti-NY-ESO-1 titers occurred in 79% (33/42) of evaluable patients, with high titers (>1:10,000) in 52% and very high titers (>1:100,000) in 33% of patients. Similarly strong humoral immunity developed in each cohort and in patients with or without confirmed NY-ESO-1 expression in their tumor. Approximately 54% of patients with NY-ESO-1 positive tumors had anti-NY-ESO-1 titers at baseline and most increased after vaccination. NY-ESO-1-specific T cell responses were absent or low at baseline, but increased post-vaccination in 56% of evaluable patients, including both CD4 and/or CD8 T cell responses. Durability of the T cell response was demonstrated in two patients from whom samples from additional cycles of CDX-1401 treatment were available. In these patients, the induction of NY-ESO-1 specific T cells was maintained through three cycles (approximately seven months) of treatment.
Thirteen patients experienced stable disease, with a median duration of 6.7 months (2.4+ to 13.4). In addition, two patients with melanoma experienced tumor regression of about 20% shrinkage in target lesions. The detection of NY-ESO-1 expression in tumor tissue did not appear to correlate with patient outcome. Stable disease was seen in 7/27 (26%) of the patients with NY-ESO-1 expression, and in 5/15 (33%) of those lacking NY-ESO-1 expression. However, the proportion of patients with stable disease was higher for those who maintained or developed NY-ESO-1 specific T cell responses. Stable disease was seen in 3/6 (50%) patients who entered the study with pre-existing cellular immunity to NY-ESO-1, and all three had increased responses while on study. For the remaining 13 patients who developed cellular immunity while on treatment, 6 (46%) experienced stable disease. In contrast, stable disease was seen in only 2/15 (13%) patients who did not develop cellular immunity to NY-ESO-1. Interestingly, 4/6 (67%) patients that displayed the strongest responses (>50 IFNγ spots per 2 x 105 PBMC) also experienced stable disease. The association of cellular response and stable disease does not appear to be a consequence of extended duration of therapy. Peak responses were observed in the first treatment cycle for seven of the nine patients with stable disease who developed cellular immunity.
Of the 45 patients in the Phase 1 study, eight went on to receive subsequent therapy of either Yervoy® or an investigational checkpoint inhibitor and six of these patients had objective tumor regression. Six patients with melanoma received Yervoy within three months of treatment with CDX-1401 and four (67%) had objective tumor responses, including one complete response, which compares favorably to the overall response rate of 11% previously reported in metastatic melanoma patients treated with single-agent Yervoy. In addition, two patients with non-small cell lung cancer received an investigational checkpoint blockade within two months of completing treatment with CDX-1401 and both achieved partial responses. All six of the responding patients had tumors confirmed to express NY-ESO-1. Interestingly, five also developed NY-ESO-1-specific cellular response, while four also developed or maintained NY-ESO-1 specific humoral response, by the end of treatment with CDX-1401.
More information: "Induction of Antigen-Specific Immunity with a Vaccine Targeting NY-ESO-1 to the Dendritic Cell Receptor DEC-205," by M.V. Dhodapkar et al, Science Translational Medicine, 2014.











