Research uncovers DNA looping damage tied to HPV cancer

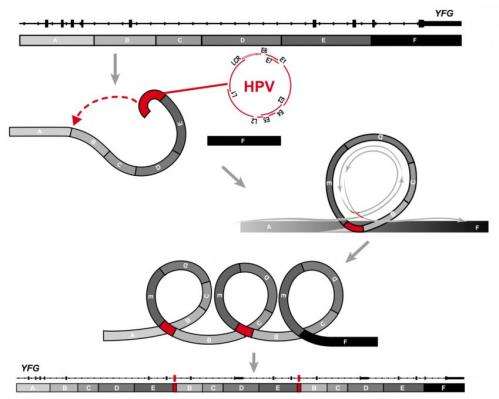
It's long been known that certain strains of human papillomavirus (HPV) cause cancer. Now, researchers at The Ohio State University have determined a new way that HPV might spark cancer development – by disrupting the human DNA sequence with repeating loops when the virus is inserted into host-cell DNA as it replicates.
Worldwide, HPV causes about 610,000 cases of cancer annually, accounting for about five percent of all cancer cases and virtually all cases of cervical cancer. Yet, the mechanisms behind the process aren't yet completely understood.
This study, recently published in the journal Genome Research, leveraged the massive computational power of the Ohio Supercomputer Center (OSC) systems. The researchers employed whole-genome sequencing, genomic alignment and other molecular analysis methods to examine ten cancer-cell lines and two head and neck tumor samples from patients – each sequence comprising the three billion chemical units within the human genetic instruction set.
"Our sequencing data showed in vivid detail that HPV can damage host-cell genes and chromosomes at sites of viral insertion," said co-senior author David Symer, M.D., Ph.D., assistant professor of molecular virology, immunology and medical genetics at Ohio State's Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James).
"HPV can act like a tornado hitting the genome, disrupting and rearranging nearby host-cell genes," he said. "This can lead to overexpression of cancer-causing genes in some cases, or it can disrupt protective tumor-suppressor genes in others. Both kinds of damage likely promote the development of cancer."
The study's first author Keiko Akagi, Ph.D., a bioinformatics expert and research assistant professor of molecular virology, immunology and medical genetics at OSUCCC – James, utilized the computational capabilities of OSC's HP-built Intel Xeon cluster. The 8,300+ cores of the Oakley Cluster offer Ohio researchers a total peak performance of 154 teraflops – tech speak for making 154 trillion calculations per second – and OSC's Mass Storage System provides them with more than 2 petabytes of storage.
"We observed fragments of the host-cell genome to be removed, rearranged or increased in number at sites of HPV insertion into the genome," said co-senior author Maura Gillison, M.D., Ph.D., professor of medicine, epidemiology and otolaryngology and the Jeg Coughlin Chair of Cancer Research at OSUCCC – James. "These remarkable changes in host genes were accompanied by increases in the number of HPV copies in the host cell, thereby also increasing the expression of viral E6 and E7, the cancer-promoting genes."
Cancer-causing types of HPV produce two viral proteins, called E6 and E7, which are essential for the development of cancer, but are not alone sufficient to cause cancer. Additional alterations in host-cell genes are necessary for cancer to develop, which is where the destabilizing loops might play a significant role; genomic instability is a hallmark of human cancers, including the HPV virus.
"Our study reveals new and interesting information about what happens to HPV in the 'end game' in cancers," Symer says. "Overall, our results shed new light on the potentially critical, catastrophic steps in the progression from initial viral infection to development of an HPV-associated cancer."















