To curb hepatitis C, test and treat inmates
Problematic as it is for society, the high incarceration rate in the United States presents an important public health opportunity, according to a new "Perspective" article in the New England Journal of Medicine. It could make staving off the worst of the oncoming hepatitis C epidemic considerably easier.
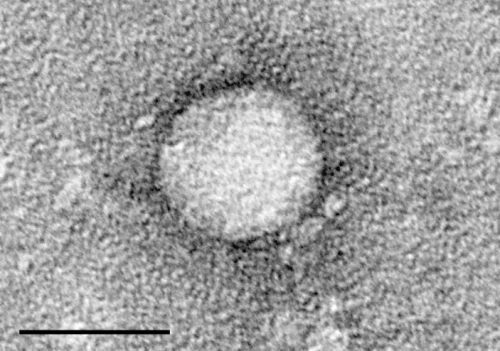
Nearly 4 million Americans may be infected with the hepatitis C virus (HCV). Many of them don't know they carry HCV, which can take decades to make them ill with cirrhosis, cancer, or liver failure. About a million people could die because of HCV by 2060, the authors wrote, and many who are saved will have required critical and costly treatments, including liver transplants.
"We know this is going to come crashing down on us," said lead author Dr. Josiah D. Rich, professor of medicine and epidemiology at Brown University and director of the Center for Prisoner Health and Human Rights at The Miriam Hospital. "It's already starting to come crashing down. The next 10 to 20 years are going to be ugly."
The single best setting for fighting the epidemic is U.S. prisons and jails, where more than 10 million people cycle through each year. In part because a major means of HCV transmission is through injection drug use, a large portion of the nation's infected population passes through the criminal justice system. In the journal, for example, Rich and his coauthors estimate that one in six inmates is infected and one in three infected Americans ends up locked up for at least a little time in their lives.
"We can head off a lot of disease and expense if we invest now," Rich said. "How do we do that most efficiently and effectively? What we're arguing in the paper is that we do it using the criminal justice system infrastructure."
Worth the considerable cost
The key barrier, Rich readily acknowledges, is the very high cost of hepatitis C drugs. A 12-week course of Sovaldi, made by Gilead Sciences, costs $84,000 a person. Treating all current inmates with HCV would therefore cost $33 billion, the authors estimate. Treating just half the people who cycle through prisons and jails in a given year would cost $77 billion.
But drug costs don't have to be nearly so high if state prison systems can negotiate reasonable discounts with drug makers, as the federal government does for its prisoners.
And while prisons have a clear disincentive to spend money to treat people who may well be released before they become sick, the money cannot and need not come solely from their budgets.
"The criminal justice system cannot be expected to shoulder the prohibitive costs of hepatitis C treatments alone," said co-author Dr. Brie A. Williams, associate professor of Medicine at the University of California–San Francisco. "Recognizing that infectious disease epidemics cannot be contained behind prison walls, we must develop a national strategy for responding to them that includes financial support and an infrastructure to test and treat prisoners, both within prisons and jails and after they return to our communities."
U.S. society as a whole will pay the costs of an inadequately addressed HCV epidemic, the authors said. Helping prisons to provide this treatment will also curb the need for litigation by prisoner advocates to a community standard of HCV care for prisoners, said co-author Dr. Scott A. Allen, professor of medicine at the University of California–Riverside.
"Even with the high cost, the drugs appear to be cost-effective," Allen said. "Private insurers in the community appear to be covering it. That establishes a clear community standard, and prisons will be held to that standard by the courts. The public policy question isn't whether or not we pay for hepatitis C care but how we pay for it."
A potential model already exists in the Ryan White Care Act, the three authors note. Congress could consider replicating that achievement of funding widespread HIV services and treatment for people who couldn't obtain them otherwise them. An HCV version could include programs and grants for prisons and jails, as well as programs to prevent reinfection of inmates after they are released.
"Seizing this opportunity for timely care will require leaders to consider the criminal justice system as part of the fabric of U.S. health care," the authors concluded. "This step will help to change the perception of the HCV epidemic in the criminal justice system, transforming it from a legal liability to a critical opportunity to change the course of HCV in the United States."















