'Antibiogram' use in nursing facilities could help improve antibiotic use, effectiveness
Use of "antibiograms" in skilled nursing facilities could improve antibiotic effectiveness and help address problems with antibiotic resistance that are becoming a national crisis, researchers conclude in a new study.
Antibiograms are tools that aid health care practitioners in prescribing antibiotics in local populations, such as a hospital, nursing home or the community. They are based on information from microbiology laboratory tests and provide information on how likely a certain antibiotic is to effectively treat a particular infection.
The recent research, published by researchers from Oregon State University in Infection Control and Hospital Epidemiology, pointed out that 85 percent of antibiotic prescriptions, in the skilled nursing facility residents who were studied, were made "empirically," or without culture data to help determine what drug, if any, would be effective.
Of those prescriptions, 65 percent were found to be inappropriate, in that they were unlikely to effectively treat the target infection.
By contrast, use of antibiograms in one facility improved appropriate prescribing by 40 percent, although due to small sample sizes the improvement was not statistically significant.
"When we're only prescribing an appropriate antibiotic 35 percent of the time, that's clearly a problem," said Jon Furuno, lead author on the study and an associate professor in the Oregon State University/Oregon Health & Science University College of Pharmacy.
"Wider use of antibiograms won't solve this problem, but in combination with other approaches, such as better dose and therapy monitoring, and limiting use of certain drugs, we should be able to be more effective," Furuno said.
"And it's essential we do more to address the issues of antibiotic resistance," he said. "We're not keeping up with this problem. Pretty soon, there won't be anything left in the medical cabinet that works for certain infections."
In September, President Obama called antibiotic resistant infections "a serious threat to public health and the economy," and outlined a new national initiative to address the issue. The Centers for Disease Control and Prevention has concluded that the problem is associated with an additional 23,000 deaths and 2 million illnesses each year in the U.S., as well as up to $55 billion in direct health care costs and lost productivity.
Antibiograms may literally be pocket-sized documents that outline which antibiotics in a local setting are most likely to be effective. They are often used in hospitals but less so in other health care settings, researchers say. There are opportunities to increase their use in nursing homes but also in large medical clinics and other local health care facilities for outpatient treatment. The recent study was based on analysis of 839 resident and patient records from skilled nursing and acute care facilities.
"Antibiograms help support appropriate and prudent antibiotic use," said Jessina McGregor, also an associate professor in the OSU/OHSU College of Pharmacy, and lead author on another recent publication on evaluating antimicrobial programs.
"Improved antimicrobial prescriptions can help save lives, but they also benefit more than just an individual patient," McGregor said. "The judicious use of antibiotics helps everyone in a community by slowing the spread of drug-resistant genes. It's an issue that each person should be aware of and consider."
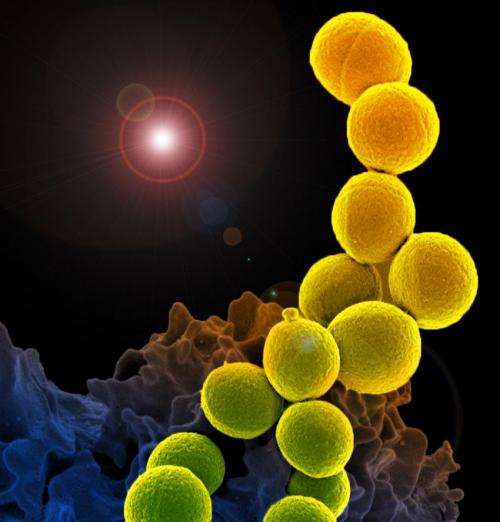
Multi-drug resistant organisms, such as methicillin-resistant Staphylococcus aureus, or MRSA, and other bacterial attacks that are being called "superinfections" have become a major issue.
Improved antibiotic treatment using a range of tactics, researchers say, could ultimately reduce morbidity, save money and lives, and improve patients' quality of life.















