Hypofractionation vs. Conventional fractionation in breast cancer radiotherapy
JAMA Oncology will publish two studies, a commentary and an author audio interview examining outcomes in women with breast cancer who had breast-conserving surgery and were treated with hypofractionated radiation therapy (shorter courses of radiation treatment administered in larger daily fraction sizes) compared with longer courses of conventionally fractionated radiation therapy.
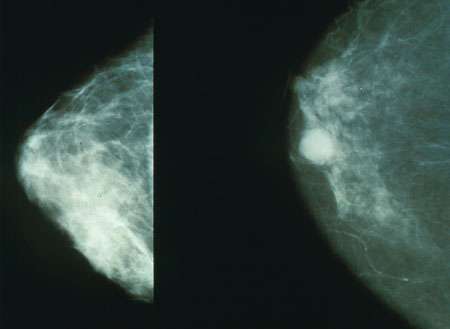
In the first article, Benjamin D. Smith, M.D., of the University of Texas MD Anderson Cancer Center, Houston1, and coauthors conducted a randomized clinical trial of 287 women to assess the acute and six-month toxic effects, as well as quality of life, associated with conventionally fractionated vs. hypofractionated whole breast irradiation. The women were 40 or older and had stage 0 to stage 2 breast cancer.
While follow-up in other clinical trials has shown equivalent rates of overall survival and local tumor control between the two treatment regimens, the adoption of hypofractionated whole breast irradiation has been slow in the United States for a variety of reasons. Only about a third of patients for whom HF-WBI (hypofractionated-whole breast irradiation) is endorsed by the American Society for Radiation Oncology actually receive the treatment, according to background in the study.
Of the 287 women, 149 were assigned to conventionally fractionated therapy (50 Gy/25 fractions plus a boost) and 138 to hypofractionated therapy (42.56 Gy/16 fractions plus a boost).
Acute dermatitis, pruritus (severe itching), breast pain, hyperpigmentation and fatigue during radiation were lower in patients with hypofractionated therapy. After six months, physicians also reported less fatigue among patients with hypofractionated therapy and patients reported less lack of energy and less trouble meeting family needs.
"In this randomized clinical trial, HF-WBI [hypofractionated-whole breast irradiation] resulted in substantially lower rates of acute and short-term toxic effects than CF-WBI [conventionally fractionated-whole breast irradiation]. These findings should be communicated to patients as part of shared decision-making regarding election of radiotherapy regimen and are relevant to the ongoing discussion regarding the most appropriate standard of care for WBI dose fractionation," the authors conclude.
In the second article, Reshma Jagsi, M.D., D.Phil., of the University of Michigan, Ann Arbor2, and coauthors conducted a complementary study that looked at data collected on acute toxic effects and patient-reported outcomes in a group of women treated with varying radiation fractionation in practices collaborating in the Michigan Radiation Oncology Quality Consortium.
All 2,604 patients who received whole-breast radiotherapy after lumpectomy for unilateral (in one breast) breast cancer were registered from October 2011 through June 2014. The authors analyzed data from 2,309 patients for whom there was a physician toxicity evaluation within one week of completing radiation therapy and at least one weekly toxicity evaluation during treatment.
Of the 2,309 patients evaluated, 578 received hypofractionation and 1,731 received conventionally fractionated whole-breast radiotherapy.
During treatment, patients who received conventionally fractionated whole-breast radiotherapy had higher maximum physician-assessed skin reactions, self-reported breast pain, fatigue, and bother from burning/stinging, hurting and swelling. However, no significant differences were seen in outcomes during follow-up through six months, according to the results.
"This study provides information about the frequency and nature of acute toxic effects during whole-breast hypofractionated radiotherapy, highly relevant to women considering this treatment and absent from the literature to date. Given the importance of patient-reported outcomes and generalizable evidence of comparative effectiveness from patients treated outside the context of clinical trials, it provides a complement to the findings of randomized trials and encourages enthusiasm for this innovative approach," the authors conclude.
In a related commentary, Shyam K. Tanguturi, M.D., the Harvard Radiation Oncology Program, Boston, and Jennifer R. Bellon, M.D., of the Dana-Farber Cancer Institute, Boston3, write: "These two studies are highly complementary. The study by Jagsi et al represents a real-world, community-based study using an impressively large cohort, albeit subject to standard confounding from its nonrandomized design. ... On the other hand, the trial by Shaitelman et al represents a more rigorous, randomized study design though limited by lower patient numbers. These studies collectively illustrate significantly lower rates of patient- and physician-reported early morbidities with hypofractionated therapy, providing critical support for this growing treatment modality. ... With comparable tumor control, lower costs and reduced morbidity, hypofractionation should be strongly considered for the majority of patients with early-stage disease."
More information: Original Investigation: Acute and Short-Term Toxic Effects of Conventionally Fractionated vs. Hypofractionated Whole-Breast Irradiation (Smith et al) JAMA Oncol. Published online August 6, 2015. DOI: 10.1001/jamaoncol.2015.2666
Original Investigation: Differences in the Acute Toxic Effects of Breast Radiotherapy by Fractionation Schedule (Jagsi et al) JAMA Oncol. Published online August 6, 2015. DOI: 10.1001/jamaoncol.2015.2590
Commentary: Hypofractionation for Early-Stage Breast Cancer (Tanguturi, Bellon) JAMA Oncol. Published online August 6, 2015. DOI: 10.1001/jamaoncol.2015.2605















