Is your doctor choosing the right IV?

When we doctors sit down with patients in the hospital, discussions regarding diagnosis and prognosis are routine. For patients who need treatments such as antibiotics or chemotherapy beyond the hospital, our conversations span how best to arrange this therapy. And often, patients put their complete trust in us by saying, "Doc, do whatever's best."
For treating infections, we know which antibiotics work and how best to administer them. Similarly, for cancer, there is much evidence regarding the optimal chemotherapy drug, dose and duration.
But when it comes to choosing the intravenous (IV) devices to deliver these treatments, what is best isn't often clear. And because there are many different kinds of IVs, the information guiding use of any one is frequently limited.
Take, for example, the case of the peripherally inserted central catheter (PICC). You might not have heard of this device, but it's use has grown rapidly in hospitals across the country. For some patients, PICCs are a great choice, but for others – less so.
What do you know about your IV?
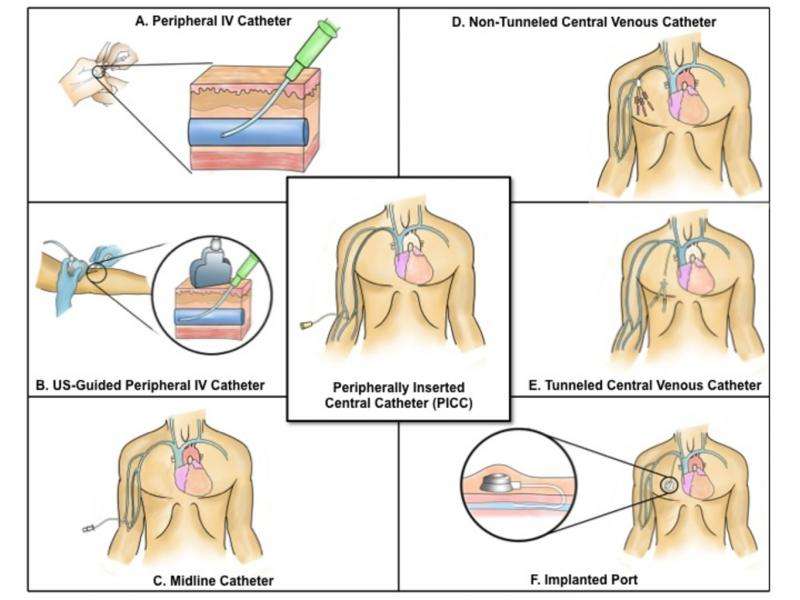
At least one billion different types of IVs are placed each year. In fact, the term "IV" covers not one, but a number of devices that come in various shapes and forms. For instance, you've probably seen or had the short peripheral IV that goes in the arm or hand. In intensive care units, longer IVs with multiple channels placed by physicians directly in the veins of the neck or chest are more common. And in patients with cancer, more elaborate IVs such as tunneled catheters or infusion ports (large IVs placed under the skin and channeled into deep veins) are preferred because they are permanent and more durable than others.
Peripherally inserted central catheters are a hybrid device. While inserted in the arm (much like a short peripheral IV), PICCs end in large veins close to the heart (like a tunneled catheter or port). Because this makes them both easy to insert and versatile for clinical needs, doctors have increasingly gravitated to using them in a wide range of patients.
Why have PICCs become so common?
Compared to a port or tunneled catheter, a PICC is a quick and easy option. Most PICCs can be placed in under an hour and on short notice either in the clinic or at the bedside, while ports or tunneled catheters involve more invasive procedures and special procedure rooms.
PICCs are designed to stay in place for weeks or months, so that patients can leave the hospital while continuing treatments in the comfort of their home.
Nowadays, trained nurses place most PICCs rather than physicians, a fact that has both reduced cost and made them a popular choice. This is a good thing, as nurses are far better than most physicians at inserting IVs – and PICCs are no exception to this rule. And in a recent study we found that approximately 70% of major US hospitals now have dedicated nursing teams to place PICCs.
The fact that PICCs are now a comparatively cheap and easy option helps explain why use of these devices has grown.
The promise and peril of PICCs
While PICCs have a lot of benefits, they (like all IVs) aren't risk-free. Studies suggest that their use may lead to complications such as blood clots and bloodstream infections. For example, a recent University of Vermont study found that more than half of all blood clots in hospitalized medical patients occurred not in the legs (where they typically develop), but rather in the arms of patients with PICCs. In another study, PICCswere associated with a greater risk of infection in critically ill patients and those with cancer, the very populations that most often receive these devices.
These data don't mean that PICCs are bad – it just means that physicians need to weigh the costs and benefits of using them carefully.
But mounting evidence suggest that physicians aren't "picking" wisely. For instance, regional and national physician surveys have reported important knowledge gaps when it comes to reasons for PICC use and management of complications. Similarly, one study of pediatric patients in a large teaching hospital found that a substantial proportion of children underwent repeated PICC removals and placements for unclear reasons, placing them at unnecessary risk for complications. And another study found that one in five doctors did not even know that their patients had a PICC, despite the fact that they requested their placement and were responsible for their care.
This is happening because research and focus on IV devices such as PICCs is underdeveloped, underfunded and understudied. Aside from the nurses who place and care for them every day, IVs are simply "invisible" to the doctors that order them. This problem isn't peculiar to the United States; concerns regarding IVs have been reported in other nations as well.
Getting picky about PICCs
Clearly physician practice for PICCs must improve. The first step to achieving this goal is to understand and quantify the extent of the problem.
Through an ongoing Blue Cross Blue Shield of Michigan-sponsored initiative, 52 Michigan hospitals are collaborating with our research team to address this very need, generating real-world data and valuable insights.
For instance, in looking at 10,000 PICCs placed within the last year, we observed that a medical reason for PICC use was not known in 20% of patients. This, while complications such as infections, blood clots and blockages of PICCs requiring prolonged antibiotics, blood thinners and clot busters occurred frequently. Even though they are intended for long-term use, we also found that one in four PICCs was removed with five days of insertion. In Michigan alone, this practice has affected thousands of patients. And collectively, these data well illustrate how much current practices must improve in order to decrease harm.
Improving the use of IVs such as PICCs will require a multi-pronged strategy. One part of the solution is to make sure physicians have guidance on choosing the right IV. To do this we brought national and international experts together with a patient and developed the Michigan Appropriateness Guide for Intravenous Catheters (MAGIC).
This first-of-its-kind document seeks to inform physicians about which IV to use and how best to prevent complications. Hospitals across Michigan will begin putting this to use in the next few months. The guideline (and associated resources) are also available to doctors, nurses, hospitals and health systems interested in improving their own IV practice.
Moving the needle forward
Choosing the right IV shouldn't be a reflex decision. Like any other treatment decision, it should be backed up by good science with careful consideration of risks and patient preference. This means we need more research comparing IV devices, and real-world registries to inform care. Without these, doctors are simply flying in the dark. Think about that when you next get an IV.
This story is published courtesy of The Conversation (under Creative Commons-Attribution/No derivatives).
![]()
















