Expensive drugs that cure hepatitis C are worth the cost, even at early stages of liver fibrosis
It is worthwhile to give patients expensive new drugs that can cure their hepatitis C much earlier than some insurers are now willing to pay for them, according to a UC San Francisco study that models the effects of treating the disease early versus late in its development.
Researchers said they were surprised by the findings, since the drugs can cost up to $100,000 for a full course of treatment. But when they factored in the long-term medical cost of delaying treatment for hepatitis C, they found the savings, in combination with improvements in the quality of patients' lives, were enough under current standards to justify using them even at early stages of liver fibrosis. Researchers said the drugs were therefore cost effective.
Cost effectiveness is a measure of broad social benefit that health economists use to make decisions about whether medical treatments are warranted. The researchers said the balance was tipped in favor of the drugs because the hepatitis C virus can cause so much damage. Hepatitis C is one of the leading causes of liver cancer, liver transplants and liver-related death, yet the drugs can prevent much of that with an early cure. Moreover, even if costly hepatitis C treatments are delayed, they eventually will be given to many patients once the infection causes enough damage to their livers.
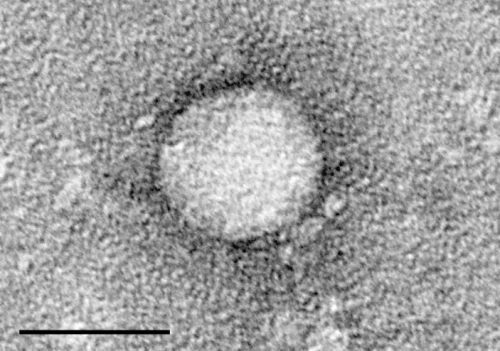
About 3.2 million people have hepatitis C in the United States. The vast majority were infected by blood transfusions before testing of blood donors became available in 1992. Today, most people get infected from injecting drugs.
Left unchecked, hepatitis C causes varying degrees of liver fibrosis in a majority of those infected, and causes cirrhosis in 20 to 30 percent. This damage is classified in five stages of increasing severity, from zero to four. Using sofosbuvir-ledipasvir, which is sold as Harvoni, and is one several new drugs for hepatitis C, researchers compared the costs of treating patients at all stages of fibrosis, zero through four, with the cost of waiting until stages three or four, which is when some patients are usually treated.
They found that, at current drug prices, treating half of those who are currently infected and are aware of their status but have not yet been treated would cost about $53 billion over five years, while treating these patients only at stages three and four would cost $30 billion. Since many of those patients are likely to be given the drugs at later stages of their disease, much of this cost is likely unavoidable, even if it gets delayed. But treating people early would at least avoid the costs of treating the damage from long-term infection. Researchers estimated the lifetime health care savings from treating all stages of liver fibrosis, compared to treating just three and four, at $3.3 billion.
"The budgetary implications of widespread treatment are quite large at current drug prices," said James G. Kahn, MD, MPH, a professor in the UCSF department of epidemiology and biostatics, as well as medicine. "However, these costs are time-limited, and they are lower than some other treatments that are less effective. In the U.S., we spend more than $140 billion a year treating cancer, often with less health benefit than is provided by the new hepatitis C treatments."
The researchers said it was important to broaden the discussion beyond cost-effectiveness, to include the price of drugs.
"The benefits of early therapy are significant, since it increases the number of healthy life years for patients and decreases their chances of getting serious liver diseases, like liver failure and liver cancer," said Harinder Chahal, PharmD, MSc, an assistant adjunct professor in the UCSF department of clinical pharmacy. "But the current prices are keeping early treatment out of reach for many patients, and this needs to be addressed."
















