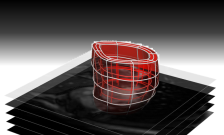
Virtual 3-D heart
Researchers at King's College London have begun a new study to help improve surgery for newborn babies with a life-threatening heart disease called hypoplastic left heart syndrome (HLHS).
This study could, ultimately, give surgeons the tools they need to select the best treatment plan for each baby, improving their chances of survival and having the best possible quality of life during their childhood and beyond.
The team will analyse MRI scans and use advanced computer modelling techniques to create a virtual 3D model of each baby's heart before and after surgery. The researchers are aiming to help doctors visualise the shape of each baby's heart at birth, provide more detailed information on the condition of each baby's heart, and help surgeons monitor how each baby's little heart adapts to surgery. The research is being funded jointly by Action Medical Research and Great Ormond Street Hospital Children's Charity with a £102,593 award.
Around one baby in every 5,000 is born with HLHS. In HLHS, the left side of the heart is much smaller than usual and cannot pump enough blood to the body. Early symptoms include difficulty breathing, a weak pulse and blueish skin. Without treatment, babies with HLHS quickly become seriously ill.
All babies affected by HLHS need a series of life-saving operations during the first few years of life. However, the severity of HLHS varies and it's not clear which surgical technique works best in each situation, for each individual baby.
In this new study researchers will analyse the MRI scans of more than 150 babies treated for HLHS. Using specially created computer techniques, researchers will then create a virtual 3D model – or avatar – of each baby's heart and its major vessel, the aorta.
These personalised models will show the shape of each baby's heart and aorta, and the way blood flows, which indicates how well the baby's heart is working. Analysing and comparing the virtual models of the heart before and after surgery will help reveal the benefits and drawbacks of different surgical techniques, and could result in personalised heart surgery for babies.
Dr Pablo Lamata, a lecturer in the Department of Biomedical Engineering at King's comments: "Babies with HLHS normally have three complex operations – the first when they're less than two weeks old. Planning these operations is difficult, because there's little evidence as to exactly which surgical technique would work best for each child at each stage. Research into the pros and cons of each technique is needed urgently. We hope that this new technique will help us determine the best approach for surgery and how babies might respond."
The treatment of babies with HLHS has already come a long way as, less than forty years ago, most babies with this serious heart defect died within weeks of birth. Improvements in surgery have given babies a much better chance of surviving but, sadly, some babies still lose their lives or are left with ongoing health problems.
Now, by personalising treatment, the team at King's College London hope to improve babies' chances of surviving and enjoying the best possible quality of life.
















