Small peptides attack ovarian cancer on two fronts, research shows
Two forms of a peptide derived from a naturally-occurring human protein can force tumors to shrink significantly in an animal model of metastatic ovarian cancer, according to a team led by researchers from Boston Children's Hospital's Vascular Biology Program, the University of Bergen and Weill Cornell Medical College. The peptides, dubbed psaptides, stimulate a response that targets tumor cells directly and also acts on the healthy tissues to make tumors' microenvironment inhospitable to metastasis. The findings suggest that psaptides could serve as a promising template for the development of treatment options directed against ovarian and maybe other cancers.
A paper outlining the research—led by co-first authors Suming Wang, PhD, and Anna Blois, PhD, of Boston Children's, and Tina El Rayes, PhD, of Weill Cornell; and senior author Randolph Watnick, PhD, of Boston Children's—appears in Science Translational Medicine.
Ovarian cancer is the fifth leading cause of cancer death among women, according to the American Cancer Society. Ovarian tumors are often clinically silent until they have spread; as a result, many women with ovarian cancer are not diagnosed until the disease has already advanced. Surgery and chemotherapy with taxanes and platinum agents are the most common therapies, but ovarian cancer cells often develop resistance to these drugs, leaving women with advanced disease few therapeutic options.
"Our goal is to develop treatments that that will cure people without making them more ill," Watnick said. "We want to find way to treat people with cancer without having to rely on cocktails of cytotoxic drugs that have significant side effects."
For the last dozen years, Watnick's laboratory has pursued that goal by attempting to understand and manipulate the microenvironment in which tumors, in particular metastatic tumors, grow and thrive. In 2009, they announced that a protein called prosaposin (psap) could block metastasis in animal models of breast and prostate cancer. Prosaposin stimulates immune cells called monocytes to produce thrombospondin-1 (TSP-1), a potent anti-angiogenic and anti-inflammatory protein that makes otherwise-permissive tissues resistant to metastasis.
Together with collaborators Lars Akslen, MD, PhD, from the University of Bergen and Vivek Mittal, PhD, of Weill Cornell, in 2013 Watnick showed that psaptide, a five-amino acid fragment of prosaposin, is fully capable of triggering TSP-1 production and could significantly reduce metastatic spread in mouse models of prostate, breast and lung cancer.
In their current study, Watnick, Akslen and Mittal sought to determine whether two modified versions of psaptide, D-psaptide and cyclopsaptide, could, via TSP-1, force established metastatic tumors to regress. D-psaptide replaces two of psaptide's amino acids with D-amino acids (mirror images of normal amino acids, which the body does not break down as readily). Cyclopsaptide is a cyclic version of D-psaptide. D-psaptide and cyclopsaptide are three and six times more potent, respectively, at stimulating TSP-1 release than native psaptide, the team found, and are also significantly more stable in human plasma.
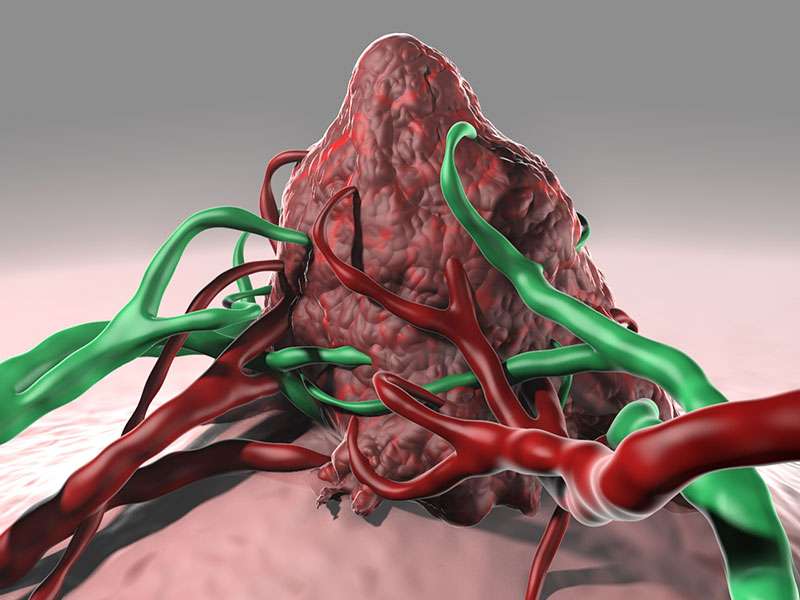
The group measured the two modified peptides' anti-tumor activities in an ovarian cancer mouse model established using patient-derived tumor cells. Ovarian cancer cells express a surface marker called CD36, a receptor for TSP-1 that, when triggered, can force ovarian cancer cells to enter apoptosis (programmed cell death).
"Essentially, we're using the prosaposin peptides as immunomodulators by getting them to turn monocytes into delivery vehicles to get TSP-1 to ovarian tumors," Watnick explained. "This strategy should work without interfering with any immune response directed specifically against the tumor."
In one set of experiments, mice received daily treatment with cisplatin or D-psaptide for up to 83 days. In a second set, the tumors were allowed to establish themselves for a longer period of time and then were treated daily with either cisplatin or cyclopsaptide and followed for a shorter period of time (15 days) to allow close examination of any remaining tumor.
The results were striking. In the cisplatin/D-psaptide comparisons, tumors regressed in mice treated with cisplatin until about day 20, at which point they became resistant and started growing again. Tumors in D-psaptide-treated animals, by contrast, regressed to the point where by day 48 they were undetectable, and remained so until the end of the experiment 35 days later.
In the cisplatin/cyclopsaptide comparison, at the end of 15 days metastatic tumors in cyclopsaptide-treated animals were 2.3 times smaller than those in cisplatin-treated animals. The team noted widespread TSP-1 expression in the tissue surrounding tumors in the cyclopsaptide mice; by contrast, TSP-1 was nearly undetectable in the cisplatin mice. Finally, 59 percent of the cells in the cyclopsaptide animals' tumors were apoptotic, compared to 11 percent in the cisplatin animals.
Taken together, the study's data form a strong body of evidence favoring exploration of psaptide-based peptide drugs.
"Many other tumors besides ovarian cancer express TSP-1's receptor, CD36," Watnick said. "It's a key receptor for tumor cell growth, and if anything, they express more of it as they become more aggressive. Hopefully we can turn that dependency against them."
More information: "Development of a prosaposin-derived therapeutic cyclic peptide that targets ovarian cancer via the tumor microenvironment," Science Translational Medicine, DOI: 10.1126/scitranslmed.aad5653













