Study finds non-narcotic nerve block controls children's pain, shortens hospital stays
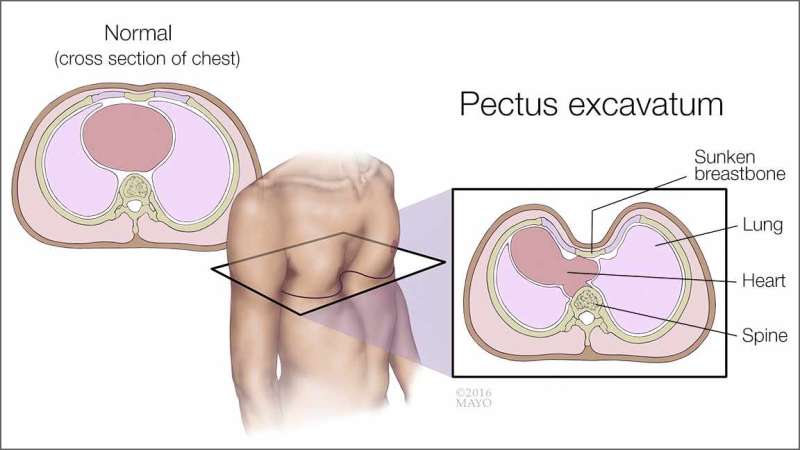
A congenital condition called pectus excavatum, in which a child's breastbone is sunken into the chest, can be corrected through minimally invasive surgery, but pain control after the operation can be a challenge. A Mayo Clinic study has found an effective way to control pain and reduce opioid painkiller use after surgery: sending children home with catheters that infuse a non-narcotic nerve-blocking drug called a paravertebral blockade. Use of the blocks shortens hospital stays and reduces opioid use after surgery, the researchers discovered. The findings were presented at the American Pediatric Surgical Association annual meeting in San Diego.
The study focused on pain control after children receive a Nuss procedure, in which small incisions are made and a stainless steel or titanium bar is placed under the sternum to reshape the chest wall. Researchers looked at the cases of 132 children who had Nuss surgery from 2010 through 2015. Of those, 114 received paravertebral catheters and continued receiving the infusions for two to five days after returning home. Eighteen were instead given an anesthetic injection called an epidural.
Use of paravertebral catheters cut the median hospital stay by roughly a day and a half from 120 hours to 80 hours, the researchers found. Opioid painkiller consumption also decreased. Opioids can have significant side effects that slow recovery after surgery, including drowsiness, lightheadedness, nausea, constipation and risk of falls.
"Our operation is minimally invasive, but it produces major changes in the chest wall. Pain was an issue for our patients, but this new technique has solved the problem. It's better than an epidural, because it's reliable, and kids can go home with it. For the first time, we consistently deliver on our promise to minimize pain," says co-author Christopher Moir, M.D., a pediatric and thoracic surgeon in the Mayo Clinic Children's Center.
Chest wall deformities are fairly common. Pectus excavatum, also called funnel chest, is the most frequent. The sunken breastbone is noticeable when a child is born and typically worsens during the adolescent growth spurt. Even mild cases can cause children to feel self-conscious. Severe cases can interfere with heart and lung function.
Physical therapy can improve posture when the deformity is mild. Surgery can correct moderate to severe cases. The most common surgery to correct pectus excavatum used to be a chest-opening procedure in which the ribcage was reshaped. More recently, the less-invasive Nuss procedure has been adopted, but it can include significant pain after surgery, and possibly more pain than the open procedure. Pain control can affect several physical outcomes after surgery, including how well a child can breathe deeply, how early a patient can walk after surgery, and the length of the hospital stay.
Epidurals have been a standard method to manage pain after pectus excavatum surgery, but they are stopped before children leave the hospital, and severe pain may persist after that. Many hospitals, including Mayo Clinic, have been using other options, such as nerve blocks, patient-controlled painkiller delivery and non-narcotic painkiller injections. There has been little consistent data on pain outcomes.
"This study puts solid data to what we see each day in the hospital and what families tell us. Paravertebal catheters work," Dr. Moir says.
Previous research at Mayo and other institutions has found that paravertebral blocks effectively control pain in operations, including breast cancer surgery, hernia repair and shoulder surgery.
















