HIV has no borders, but its treatment does—why this needs to change
Panashe is a 26-year-old Zimbabwean woman living with HIV. She works in a restaurant on the western peripheries of Johannesburg.
She has known she is HIV positive since she was 20 years old living in Harare, Zimbabwe. This is where she started her antiretroviral treatment. She takes her antiretrovirals religiously and without problems. But this was not always the case.
When Panashe moved from Zimbabwe to South Africa in 2012 as an asylum seeker, she encountered problems with her treatment. Continuing treatment in the new country was a challenging and disorienting affair.
Antiretroviral treatment has been freely available in South Africa since 2007 and asylum seekers and refugees are eligible for treatment. But when Panashe arrived in South Africa, she was forced to change her treatment regimen. Antiretroviral regimens are the drug combinations people living with HIV are put on. The specific regimen depends on the antiretrovirals that the country makes available.
The forced regimen change meant that she had severe side effects which made her sick and nearly made her stop taking medication – a move which would have compromised her health. After a few weeks she adapted to the change, but her challenges reveal a wider problem.
The change happened because there are no regionally implemented and adopted treatment guidelines or referral systems for cross-border migrants who need antiretrovirals.
South Africa and Zimbabwe have made significant strides rolling out antiretroviral programmes. But Panashe's story shows that the regional expansion of antiretroviral programmes still needs much work and needs to integrate migration.
This requires the regional harmonisation of treatment regimens and protocols and for regional referral systems to be developed. These systems should provide information about the possibilities of HIV treatment across borders at a clinic level and inclusion of foreign nationals into local support groups.
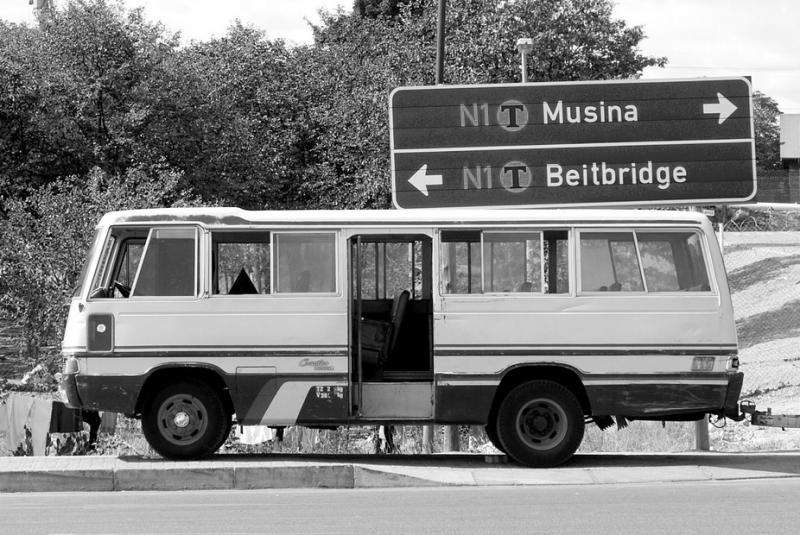
Crossing the border
Our ongoing research has been looking at the links between health and migration across borders in the southern Africa region. As part of our research we have spoken to government officials, researchers, funders and non-governmental organisations.
We found that despite the economic and political challenges in Zimbabwe over the past two decades, it has a relatively well functioning and expansive antiretroviral programme. There are some challenges, in particular delays in starting treatment.
But more than 1500 sites offer antiretrovirals and treatment for the prevention of mother to child transmission of HIV.
There are about 1.4 million people living with HIV in Zimbabwe, compared to around seven million in South Africa. About 62% of people who are eligible for treatment take antiretrovirals. This is better than South Africa where only 48% are on medication.
There is no reliable data on migrants accessing or needing antiretrovirals in South Africa or the countries in the Southern African Development Community. But there are both Zimbabweans going to South Africa and Zimbabweans returning home. These migrants encounter three main challenges with cross border treatment.
Firstly, there is no standardised referral system. This means that cross-border migrants are sometimes unable to continue with the same treatment and are forced to change treatment regimes. They may risk missing treatment while registering in a new system.
Missed treatment or poor adherence and management of treatment can lead to the development of drug resistant strains of HIV which contributes to treatment failure.
This relates to the two other problems: changes in treatment and a lack of information.
Regimen changes are possible but can be daunting for people living with HIV on treatment. Treatment regimens in the region are very similar and changes can be managed effectively. But regimen changes can produce changes in side effects, and ordinarily require intensive monitoring.
Ordinarily, treatment regimen change is made in cases where there is viral resistance to a particular regimen, or when side effects are particularly severe.
Thirdly, information provided to patients about moving treatment sites across borders is scarce. Often providing additional pills in case of mobility is left to the discretion of doctors, and little information is provided about how to go about transfers.
Cross-border migrants often do not know how to negotiate foreign systems, and sometimes have to deal with xenophobia in clinics.
Some progress
The Southern African Development Community is yet to harmonise treatment protocols which could improve HIV services for migrants.
In the last 10 years there have been ongoing regional policy discussions. There has been a significant movement towards regional harmonisation but there are still challenges.
There is the 2009 Policy Framework for Population Mobility and Communicable Diseases in the SADC Region. It calls for coordinated cross-border referral services and mechanisms for continuity of care for patients with communicable diseases. Diseases which require prolonged treatment such as TB and HIV are recognised as particularly important.
But these guidelines have not been adopted and implemented at a regional level.
South Africa's national Department of Health has been working on a new internal referral policy which would also address cross-border referrals, but is also yet to be implemented.
The policy should ensure that patients don't miss treatment when travelling or migrating and that migrants are supported with treatment continuation when, and if, they return home.
For Panashe, this would make decisions about her future far easier. For now, however, she fears having to change her treatment again and lacks information on how she would transfer her treatment back to Zimbabwe.
This article was originally published on The Conversation. Read the original article.![]()
















