Why a standard treatment for the aggressive blood-cell cancer AML so often fails
An international team of researchers has shown why a standard treatment for the aggressive blood-cell cancer AML so often fails. The study uncovers a new biomarker that predicts the efficacy of the chemotherapy and identifies a new drug target.
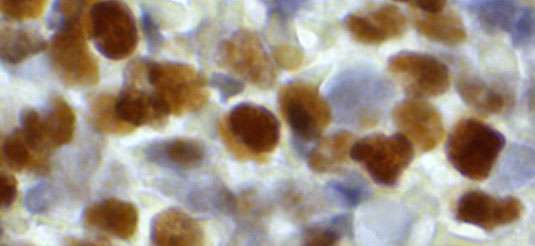
Acute myeloid leukemia (AML) is a cancer that is characterized by the uncontrolled proliferation of certain types of white blood cells. The disease results from a wide range of mutations and prognosis varies correspondingly between different patient groups. The standard therapy for all groups includes treatment with cytosine arabinoside (cytarabine), which is a so-called nucleoside analog. Most patients initially respond to chemotherapy, but many patients fail in the long run or even become resistant to the agent. Resistance results in relapse and the resumption of disease progression. Now a study led by Oliver T. Keppler, who holds the Chair of Virology at LMU's Max von Pettenkofer Institute, and Jindrich Cinatl Jr., a professor at the Institute for Medical Virology at Frankfurt University (of which Keppler was the Director before he moved to LMU in 2015) has identified the mechanism behind resistance to cytarabine.
Cytarabine is rapidly taken up by cells and is chemically modified by the addition of a so-called triphosphate moiety, a small chemical group. In fact, the modified form of the drug is the therapeutically active substance. Upon incorporation into the genome of the replicating cancer cell, it inhibits further DNA synthesis during cell division. Malignant cells in general divide very rapidly and are thusare more susceptible to its detrimental effects than most other cell types in the body. The new study, which appears in the leading journal Nature Medicine, identifies the enzyme SAMHD1 as an inhibitor of the action of cytarabine, and demonstrates that it acts by removing the triphosphate from the active drug.
Context-dependent roles
Oliver Keppler's research actually focuses on mechanisms that lead to the development of AIDS following infection with Human Immunodeficiency Virus 1 (HIV-1). So he was already familiar with SAMHD1 in the context of antiretroviral therapy, which also involves nucleoside analogs. In order to replicate successfully in human cells, HIV-1 must first convert its RNA genome into DNA via a process called reverse transcription. Like DNA replication, reverse transcription of RNA can be disrupted by the incorporation of a nucleoside analog into the growing HIV-1 DNA strand. Without intact copies of viral DNA, no new virus particles can be produced. In this case, SAMHD1 is thought to promote the inhibition of virus replication by degrading the normal DNA building blocks that the virus needs.
The LMU researchers and collaborators in Frankfurt first assumed that a similar mechanism might be at work in AML cells treated with cytarabine, and that SAMHD1 would enhance the effect of the analog. But as it turned out, exactly the opposite happens. "To our surprise, we found that the activated form of cytarabine is itself a substrate for SAMHD1," says Keppler: The enzyme deactivates the drug, thus inhibiting its ability to inhibit DNA synthesis. "Moreover, there are indications that the enzyme may also interact in the same way with triphosphates of other nucleoside analogs used in tumor therapy. In collaboration with a large group of clinicians, pathologists, pharmacologists, biochemists and biostatisticians, Keppler and his team went on to show – based both on mouse models of AML and retrospective investigations of AML patients – that SAMHD1 is indeed a crucial factor in the failure of cytarabine therapy for this type of leukemia. As the authors state in the new paper, SAMHD1 provides a cellular biomarker with which to assess the potential efficacy of therapies based on nucleoside analogs and plays a significant role in the progression of AML in individual patients. Further studies may point to ways of inhibiting the activity of SAMHD1 itself, which would be expected to boost the effectiveness of an important class of anti-tumor drugs.
More information: Constanze Schneider et al. SAMHD1 is a biomarker for cytarabine response and a therapeutic target in acute myeloid leukemia, Nature Medicine (2016). DOI: 10.1038/nm.4255













