Virtual reality in medicine—new opportunities for diagnostics and surgical planning
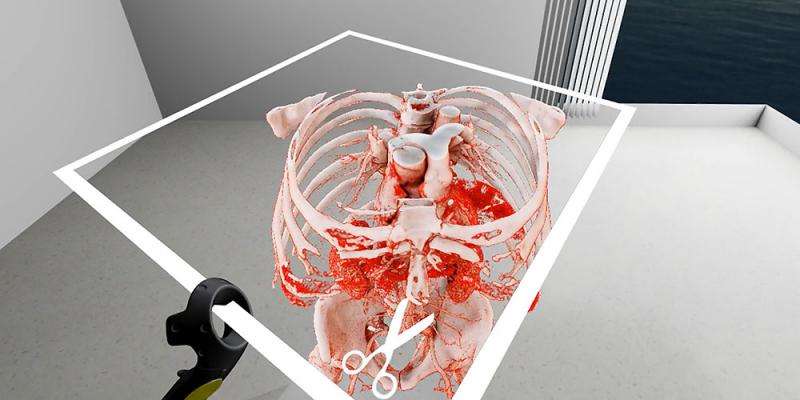
Before an operation, surgeons have to obtain the most precise image possible of the anatomical structures of the part of the body undergoing surgery. University of Basel researchers have now developed a technology that uses computed tomography data to generate a three-dimensional image in real time for use in a virtual environment.
The planning of a surgical procedure is an essential part of successful treatment. To determine how best to carry out procedures and where to make an incision, surgeons need to obtain as realistic an image as possible of anatomical structures such as bones, blood vessels, and tissues.
Researchers from the University and University Hospital of Basel's Department of Biomedical Engineering have now succeeded in taking two-dimensional cross-sections from computer tomography and converting them for use in a virtual environment without a time lag. Using sophisticated programming and the latest graphics cards, the team led by Professor Philippe C. Cattin succeeded in speeding up the volume rendering to reach the necessary frame rate. In addition, the SpectoVive system can perform fluid shadow rendering, which is important for creating a realistic impression of depth.
For example, doctors can use the latest generation of virtual reality glasses to interact in a three-dimensional space with a hip bone that requires surgery, zooming in on the bone, viewing it from any desired angle, adjusting the lighting angle, and switching between the 3-D view and regular CT images. Professor Cattin explains the overall benefits: "Virtual reality offers the doctor a very intuitive way to obtain a visual overview and understand what is possible."
"This brand-new technology smoothly blurs the boundary between the physical world and computer simulation. As a doctor, I am no longer restricted to looking at my patient's images from a bird's eye view. Instead, I become part of the image and can move around in digital worlds to prepare myself, as a surgeon, for an operation in detail never seen before," says ophthalmologist Dr. Peter Maloca.
"I have found that these new environments continue to guide me and have helped rewire my senses, ultimately making me a better doctor. Those who stand to gain the most here are doctors, their patients, and students – all of whom can share in this new information," adds Maloca, who works at University Hospital Basel's OCTlab and at Moorfields Eye Hospital in London.
Improved volume rendering
The ability to convert CT images into a 3-D on-screen representation is nothing new. Until now, however, commonly available hardware could not generate these three-dimensional volumes in real time for use in virtual spaces. One particularly challenging aspect was that smooth playback in a virtual environment requires at least 180 images a second – 90 images each for the left and right eyes; otherwise, the viewer may experience nausea or dizziness.
Widespread interest in innovation
This achievement was aided by developments in the computer games industry and new generations of powerful standard hardware, providing medical practitioners with access to three-dimensional test environments. At present, the Basel-based researchers are conducting regular demonstrations of SpectoVive to physicians in order to highlight the system's potential and, at the same time, to gain a better understanding of doctors' requirements.
Some museums have also expressed interest in the technology, seeing SpectoVive as an opportunity to allow visitors to discover the world inside exhibits, such as mummies, in an intuitive and nondestructive manner. However, Philippe Cattin, Professor for Image-Guided Therapy at the Faculty of Medicine, sees the greatest potential in the areas of diagnostics, surgical planning, and medical training.
SpectoVive – part of the MIRACLE project
This innovation is part of the MIRACLE project underway at the Department of Biomedical Engineering. The project is receiving CHF 15.2 million in funding from the Werner Siemens-Foundation. Its aim is to allow the minimally invasive treatment of bones using laser beams. One day, it is expected that SpectoVive technology will be used in the planning of surgical procedures and for the navigation of the robot-guided laser system.



















