Researchers discover new subtype of cervical cancer
A team of University of South Carolina scientists led by Carolyn Banister and Phillip Buckhaults has identified a new subtype of cervical cancer that, like most cervical cancers, is triggered by human papillomavirus (HPV) but whose growth is not directed by the virus, suggesting that therapy targeting these tumors' distinct genomic pathways may improve patient outcomes over standard treatment.
"Cervical cancer patients are currently treated as a uniform group based on chemotherapy and radiation regimens that help the largest percentage of people; however, one third of these patients are not helped by standard therapies," Banister said. "We have discovered the existence of a subgroup of cervical cancers with very different genetic features. These women may benefit from alternative treatments that are not usually given to cervical cancer patients."
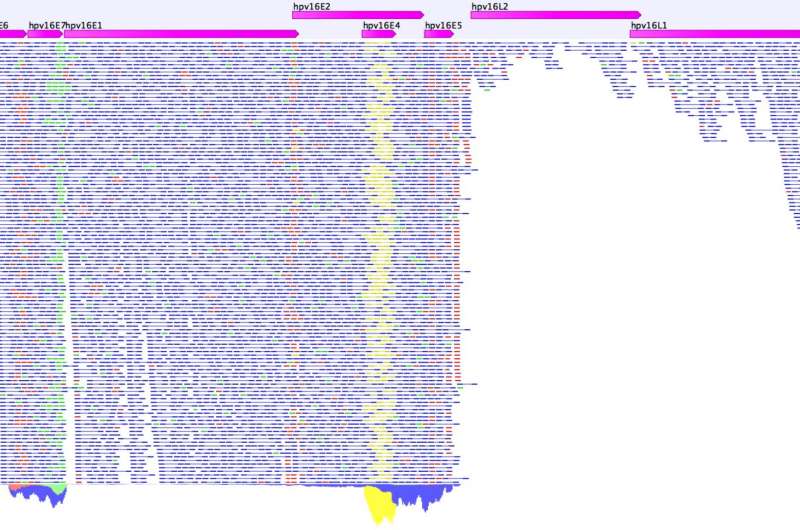
By analyzing data from 255 cervical cancer samples in The Cancer Genome Atlas—a large-scale federally funded project launched in 2005 by the National Cancer Institute and National Human Genome Research Institute—researchers from the University of South Carolina College of Pharmacy and School of Medicine found that two HPV oncogenes thought to be necessary for cervical cancer growth were expressed either at high levels (HPV-active class) or at low or zero levels (HPV-inactive class) in cervical cancer. The study was published online Jan. 6 in the journal Oncotarget.
Previous studies by the University of South Carolina's Lucia Pirisi-Kim Creek research group had reported the existence of an HPV-inactive class in head and neck cancers and raised the possibility that HPV-inactive cervical cancers might originate as virally driven cancers and subsequently act independent of HPV. This work confirmed these suspicions and discovered novel molecular genetic mechanisms driving the evolution of HPV-inactive cancers.
In addition to HPV oncogene expression, the researchers noted other distinct differences between the HPV-inactive and active classes of cervical cancers. They found significant differences in median age of diagnosis (54 years vs. 45 years, p = 0.02), median survival (715 days vs. 3,046 days, p = 0.0003), DNA methylation and gene expression profiles, and distribution of tumor cell type, with adenocarcinomas more common in HPV-inactive tumors than in HPV-active tumors (p = 0.00022).
The researchers also analyzed the somatic mutation frequencies of all human genes. They found that 19 cancer driver genes had significantly higher mutation rates in the HPV-inactive class than in the HPV-active class. These differences indicate that these mutated genes replace functions normally provided by the HPV oncogenes in regulating tumor cell growth.
For example, HPV-inactive tumors were 17 times more likely to contain disrupting TP53 gene mutations than HPV-active cervical cancers, rendering unnecessary the expression of the HPV E6 oncogene. The authors suggest that therapies targeting TP53 mutations may yield better clinical outcomes for patients with HPV-inactive tumors.
"Physicians managing cervical cancer patients should test for HPV oncogene expression in these tumors and consider personalized treatment depending on HPV activity," Banister said. "HPV-active tumors have high expression of immunoregulatory genes and therefore may respond to immune checkpoint inhibitor therapy. In contrast, HPV-inactive tumors often have mutations in the PIK3CA/PTEN/AKT pathway, indicating that AKT kinase inhibitors may be effective treatment options for these patients."
More information: Carolyn E. Banister et al, Identification and characterization of HPV-independent cervical cancers, Oncotarget (2017). DOI: 10.18632/oncotarget.14533















