Clostridium difficile infections linked to higher death rates if infection recurs
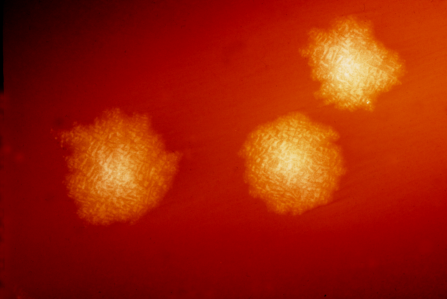
Repeated infection with the bacterium Clostridium difficile (C. difficile), which causes stomach upsets and diarrhoea, is linked to higher death rates, as well as having a significant impact on health services in terms of cost and hospital beds occupied.
In the first of two presentations at the 27th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) tomorrow (Saturday), Professor Alistair Leanord, from Glasgow University, UK, will say that in Scotland the extra impact on the health service from C. difficile infections amounted to 10,600 bed days a year. "This is the equivalent to a 30-bed hospital ward being fully occupied all year," he will say.
He will tell the congress that the (median) average cost of a patient with C. difficile infection was £7,500 (€8,600 approximately) compared to £2,800 (€3,200 approx) for patients with other medical conditions. In Scotland over a one year period, from October 2015 to October 2016, there were 1,150 cases of C. difficile infection in patients aged 15 and over. This cost the National Health Service (NHS) in Scotland a total of £8,650,000. Out of this amount, the additional costs of treating C. difficile infection, over and above the basic cost of a hospital bed and normal medical care, was £1,955,000. The calculations were carried out at Strathclyde University, which is part of the Scottish Healthcare Associated Infection Prevention Institute (SHAIPI) research consortium.
Until now, little has been known about the impact on health service resources from C. difficile infections, and on patients in terms of recurrence of infection, readmission to hospital, length of stay and death rates.
Prof. Leanord and his colleagues in Scotland identified 3,304 patients with C. difficile in Scottish hospitals between 2010 and 2013 and matched them with 9,516 patients who did not have the infection (the control group). Approximately two-thirds of the C. difficile patients acquired the infection in hospital.
They found that patients with C. difficile infection had more than double the risk of dying from any cause within two months of being admitted to hospital; nearly a third of all C. difficile cases (29%) died within two months compared to 14% of patients in the control group. Patients with C. difficile stayed in hospital a (median) average 9.7 days longer than the patients without the infection. Of the 1,712 C. difficile patients who were discharged from hospital within 30 days of the first episode of infection, 59% were readmitted within six months; of the 626 cases discharged more than 30 days after the first episode 53% were readmitted within six months. Few of these readmissions were directly related to C. difficile infection.
"However, nearly a sixth of patients (14%) who were cured of the initial infection recurred within three months, and nearly one third of them (29%) had a second recurrence within a year," says Prof. Leanord.
Older people were more vulnerable to a recurrence. Among the patients with C. difficile infection, 22% were aged 85 or over, and patients aged 75 and over had approximately double the risk of a recurrence of the infection compared to those aged under 65. Patients aged between 65-74 had 1.5 times the risk of recurrence compared to younger patients.
Prof. Leanord will conclude: "Having a clear understanding of the nature of C. difficile infections in Scotland will allow the Scottish government to target resources at the most appropriate patients to try to reduce the overall burden of the disease on the health service. Our findings are very likely to be applicable to the rest of the UK and other countries as well."
In a second presentation on Saturday, Dr David Enoch, a consultant microbiologist and infection control doctor at the National Infection Service, Public Health England, Cambridge (UK), will report the outcomes of 6,874 patients who had acquired C. difficile infection in hospital between 2002 and 2013 in England. Of these, 1,141 (16.6%) had recurrences of the infection.
"We found that 49% of hospital patients who suffer a recurrent episode of C. difficile infection die within a year, compared to 38% of those who suffer an initial infection only," he will say. "In addition, 21% of patients with a recurrence suffered other complications as well, such as dehydration, malnourishment and sometimes even perforation of the bowel, compared to 18% of patients who did not have a recurrence."
Dr Enoch estimates that there are approximately 125,000 cases of C. difficile infection in Europe each year, and between 15-30% of these recur. "Cases in the UK have been coming down since 2008, which is most probably due to improvements in antibiotic prescribing and cleaning regimens in hospitals. This is encouraging but more still needs to be done."
The average age of the patients was 77 and the average length of stay in hospital was 38 days.
"The main risk factor for developing C. difficile infection is prior antibiotic use. These patients are often already ill from some other underlying illness, which explains why they needed antibiotics in the first place. Older people are at greater risk of C. difficile infection as they are often sicker, have other illnesses or conditions, and so need more antibiotics," he will say.
Dr Enoch continues: "Although much has been done, particularly in the UK, to try to prevent C. difficile infection, strict adherence to antibiotic guidelines by clinicians and thorough cleaning of the hospital environment are crucial in ensuring that patients don't develop C. difficile infection in the first place. Treatment with a new drug called fidaxomicin has also been shown to reduce the risk of recurrence in patients who are unfortunate enough to develop an infection. However, we still have a lot to learn, particularly about how C. difficile infection occurs in the community, and how best to treat it."
Treatments for recurrences of C. difficile infection include stopping the antibiotic that made the patient susceptible to the infection and starting a different antibiotic that is effective against C. difficile infection. These antibiotics include metronidazole, vancomycin and fidaxomicin. Supportive therapy, such as extra fluids, and surgery in serious or life-threatening cases may also be necessary. Faecal transplantation is emerging as a promising option; this is a process in which the good bacteria that the gut needs but which has been killed off by antibiotics is transplanted into the patient from a healthy donor.
More information: Abstract no: #1672, presented by Prof. Alistair Leanord in the "Clostridium difficile infections: epidemiology and outcome" oral session, 16.30-18.30 hrs, Saturday 22 April, Hall A.
Abstract no: #883, presented by Dr Enoch in the "Clostridium difficile: guts and glory" e-poster mini-oral session, 15.30-16.30 hrs, Saturday 22 April, ePoster Arena 4.

















