Th17 cells could facilitate wider clinical use of adoptive immunotherapy
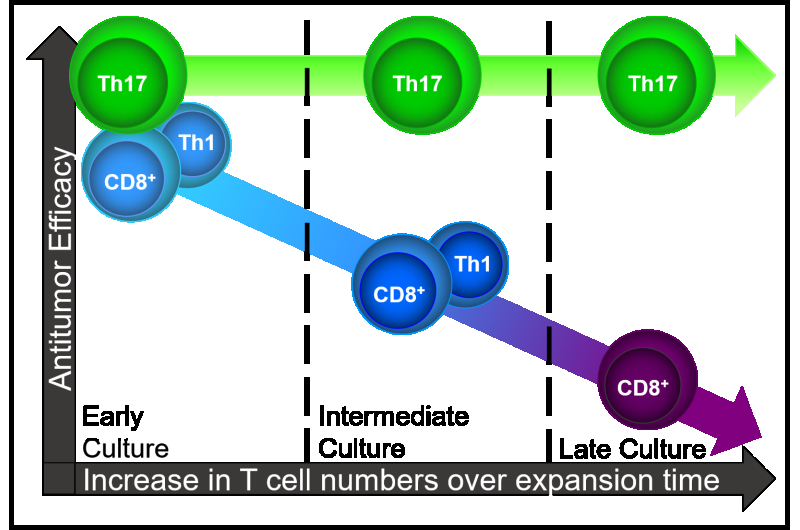
Medical University of South Carolina (MUSC) investigators report that long-term expansion protocols for adoptive cancer immunotherapy do not compromise Th17 cells' effectiveness against large tumors, in the March 9, 2017 issue of JCI Insight. This finding is important because rapid expansion protocols (REPs) that are used to produce sufficient CD8+ T cell numbers for adoptive cell therapy (ACT) degrade their effectiveness. These findings underscore that Th17 cell durability offers promise for next-generation ACT trials.
ACT is highly effective at activating the body's immune defenses to fight cancer. This immunotherapy involves extracting, expanding, and enhancing the patient's own T cells before returning them to the patient where they can induce a durable antitumor response. In fact, among metastatic melanoma patients treated with ACT, approximately 54 percent achieve an objective response and 24 percent achieve complete remission.
However, infusion of large numbers of T cells is required to produce successful antitumor responses. Rapid expansion protocols meet this need but take up to three months before enough tumor-reactive T cells are available to effectively treat cancer patients. In addition, the CD8+ T cells commonly used in clinical trials quickly lose potency when they are extensively expanded outside the body.
Preclinical studies by an MUSC research team led by Chrystal Paulos, Ph.D., associate professor of Microbiology and Immunology and Endowed Peng Chair of Dermatology and including MSTP student Jacob Bowers, demonstrate for the first time that one T cell subset, Th17 cells, is resistant to expansion-induced degradation. They found that Th17 cells circumvented rapid expansion problems, had potent antitumor activity and provided an attractive alternative to the CD8+ T cells traditionally used for ACT.
"In contrast to CD8+ or Th1 cells, we discovered Th17 cells could be expanded to large numbers without compromising their therapeutic quality," Paulos explains. "Th17 cells have a natural propensity to logarithmically expand without restimulation. And, if we did restimulate them, this approach didn't dramatically impair the antitumor response as with CD8+ T cells. Our findings have major implications for advancing the field of cancer immunotherapy."
Because Th17 cells have stem-cell-like properties (i.e., stem memory) and durable efficacy in mice, the team hypothesized that they would retain their potent antitumor effectiveness after long-term expansion outside of the body. Their experiments showed that, without restimulation, Th17 cells robustly expanded for 21 days outside the body—producing approximately 5,000 times the original number of CD4+ cells to be returned to the patient.

Furthermore, the stem memory signaling of the Th17 cells remained intact. They resisted degradation (senescence) and remained capable of eliminating melanoma in mice after two weeks of expansion outside the body—something that Th1 and CD8+ T cells could not accomplish.
In addition, Th17 cells expanded for 14 days showed the same ability to persist in the tumor-bearing host after reinfusion as those expanded for only 7 days. "Cytotoxic CD8+ or Th1 cells were less effective at clearing tumor while the Th17 cells persisted much longer," says Paulos. "The durability of Th17 cells is due, in part, to their resistance to apoptosis ) and senescence," says Paulos.
Further studies revealed that, while one week of expansion did not produce sufficient numbers of Th17 cells to effectively eradicate large, aggressively growing tumors, treatment with larger quantities of Th17 cells obtained after two to three weeks of expansion rapidly and completely eradicated these cancers in mice.
"We wanted to know whether long-term cultured cells were different than short-term cultured cells in the face of a very large tumor burden that simulates late-stage cancer," explains Paulos. "In just two weeks, we expanded enough Th17 cells to eradicate tumors and they mediated durable responses. Large Th17 cell numbers cured all the mice. When we rechallenged the same animals with another lethal tumor dose, these mice were protected but the control mice died quickly. Then we came back again 100 days later and gave these mice lung tumors and they were all still protected many months later."
Data show that Th17 cells produced this remarkably potent antitumor response by directly lysing the tumor itself. In all experiments, Th17 cells produced antitumor immunity that was superior to that obtained with classic CD8+ cells or CD4+ subsets such as Th1 cells.
These findings are important for immunotherapy product development because Th17 cell durability provides a larger window for obtaining effective, potent T cells via expansion outside the body. Th17 cell resilience could also facilitate simplified clinical trial protocols—making preparation of ACT T cells easier for cancer centers around the world and extending the benefits of ACT to more patients.
More information: Jacob S. Bowers et al, Th17 cells are refractory to senescence and retain robust antitumor activity after long-term ex vivo expansion, JCI Insight (2017). DOI: 10.1172/jci.insight.90772
















