Knowing HIV levels are 'undetectable' may affect sexual behavior
Understanding and responding to behavioral trends in groups that are at high risk for HIV infection is critical to the development of effective strategies that decrease HIV incidence and improve access to care. New research based on data from the Centers for Disease Control and Prevention's National HIV Behavioral Surveillance (NHBS) system are presented in a special supplement to JAIDS: Journal of Acquired Immune Deficiency Syndromes. The journal is published by Wolters Kluwer.
"NHBS is able to guide local and national high-impact prevention strategies by identifying who is highest risk, what they are doing, and what services they need most," according to an introduction by Cyprian Wejnert, PhD, and colleagues of the NHBS Study Group.
NHBS Data Helps to Guide HIV Prevention in High-Risk Groups
The NHBS is an ongoing surveillance project that monitors behavioral risk factors, HIV testing behaviors, and use of prevention services and strategies in three high-risk groups: men who have sex with men (MSM), persons who inject drugs (PWID), and heterosexuals of low socioeconomic status in urban areas. "Accurate data on the behaviors in these populations are critical for understanding trends in HIV infection and planning and evaluating effective HIV prevention activities," Dr. Wejnert and coauthors write.
The special issue presents 21 new research papers using NHBS data to evaluate and inform HIV prevention efforts. Among the findings are insights into HIV testing trends; recent declines in HIV diagnoses among African-American women; new evidence on the effectiveness of syringe services programs to reduce high-risk behavior among PWID; and examples of innovative programs developed to reach high-risk groups in communities across the United States.
A study by H. Fisher Raymond, DrPH, of the San Francisco Department of Public Health looks at interactions between HIV prevention efforts and sexual risk behaviors among MSM with known HIV infection. In the past decade, San Francisco has introduced a "Treatment as Prevention" (TasP) approach, in which people are started on antiviral drugs as soon as their HIV infection is diagnosed.
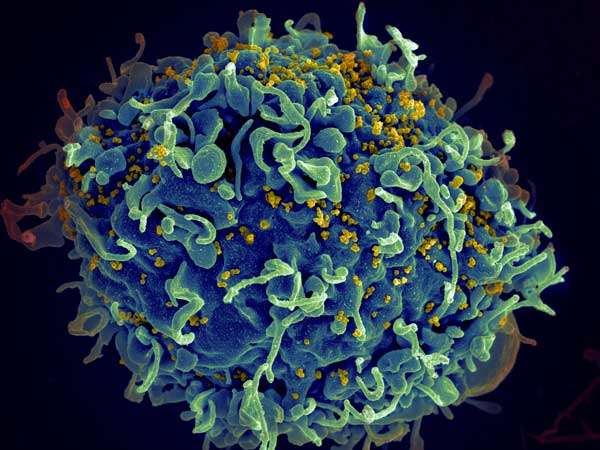
When taken the right way, every day, antiviral drugs reduce the amount of HIV in the blood and elsewhere in the body to such low levels that viral activity, measured as viral load, can no longer be detected. This is called undetectable viral load, or viral suppression. Suppressing HIV in the blood to "undetectable" levels has many health benefits. It helps people living with HIV live longer, healthier lives and dramatically reduces the risk of transmitting HIV.
Of 68 men included in the study, 58 believed they had undetectable HIV levels while nine believed they had detectable levels. In both groups, blood tests showed that 97 percent of men accurately knew their viral status.
Knowing one's viral suppression status appeared to be associated with differences in sexual risk reduction strategies.
The results suggest that MSM who have achieved viral suppression on treatment—knowing that they have a low risk of transmitting HIV—may adapt their sexual practices accordingly. The authors point out that the observed difference was not statistically significant, likely due to the small size of the study.
"More research is necessary to assess how HIV-positive men account for viral load in sexual decision-making practices, and this research many inform resource allocation and clinical recommendations to maintain the health of MSM populations," Dr. Raymond and coauthors write. They note their study doesn't reflect newer risk-reduction strategies—especially pre-exposure prophylaxis (PrEP), in which uninfected people who are at risk of HIV take medications to reduce their risk of becoming infected.
"The papers in our NHBS supplement point out that we are in a new era of HIV treatment and prevention, given the clear effects of treatment on transmission and the clear benefits of PrEP," comments Paul A. Volberding, MD, of University of California San Francisco, Editor-in-Chief of JAIDS. "This is an excellent time to record where we stand and to develop plans for continued surveillance."


















