Study shows how an opportunistic microbe kills cancer cells
New study results show for the first time how dying cells ensure that they will be replaced, and suggests an ingenious, related new approach to shrinking cancerous tumors. A research team from Rush University Medical Center will publish a new paper this week in the journal Developmental Cell that describes two groundbreaking discoveries.
"I believe this discovery is going to have important ramifications on cancer biology and cancer drug development, and on the treatment of other diseases such as diabetic foot ulcers," says Sasha Shafikhani, PhD, associate professor of Hematology, Oncology and Cell Therapy at Rush Medical College, who headed up the study.
The team made its two-pronged discovery while investigating how an opportunistic microbe kills cancer cells. For years, Shafikhani's lab has been studying Pseudomonas aeruginosa, a bacterium that can be lethal, but only to people who are already wounded or sick. This pathogenic bacterium secretes several toxins that allow it to cause infection. One such toxins, ExoT, inhibits cell division and can severely impede wound healing, but it's also known to kill cancer cells.
The researchers were trying to figure out ExoT's lethal mechanisms against cancer when they unlocked, almost by accident, a mystery researchers have been trying to solve for years, Shafikhani says. For at least 20 years, medical researchers have wondered how cells, before they die in the normal process of apoptosis, manage to alert their neighbors of the need to replace them and compensate for their demise, so to ensure the organism's survival. While shining a light on the lethal habits of Pseudomonas aeruginosa, Shafikhani's team discovered what actually happens in that "compensatory proliferation signaling" (CPS) process.
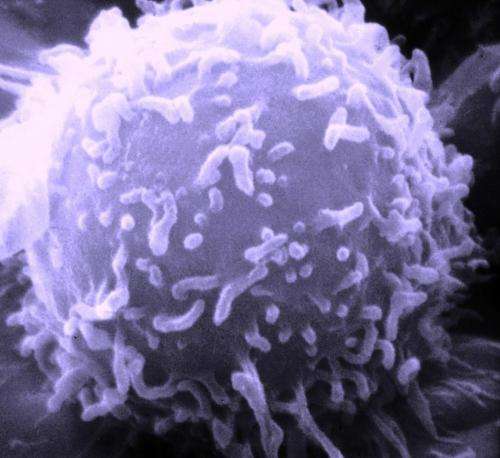
For the first time, the investigators saw—and have shown in amazing videos they produced—that during CPS, dying cells release "microvesicles" containing the CrkI protein, which travel to neighboring cells and cause them, upon contact, to create new cells to replace the ones that are dying.
Apoptosis is part of life. "In the course of normal tissue turnover in humans, about one million cells die every second, through a highly-regulated process of apoptotic programmed cell death (PCD)," the new paper states. Apoptosis is not the only type of cell death, and not all cells dying of apoptosis are capable of CPS.
Not only that, but Shafikhani and his colleagues have demonstrated that if they knocked out the CrkI protein during CPS, either genetically or with the ExoT toxin, they could stop cell compensatory proliferation cold. That's a trick P. aeruginosa uses to take advantage of damaged tissues, but it has exciting possibilities for disease treatment as well.
Apoptosis is of particular interest to cancer researchers because majority of the current cancer drugs kill cancer cells by apoptosis.
However, CPS can dog apoptosis in cancer treatment. Yes, treated cancer cells can be induced to die, but before they do, they call on nearby cancer cells to replace them, so the drug loses its effectiveness and the tumor persists. But if the communication between the dying cancer cells and neighboring cancer cells is blocked, Shafikhani says, the hope is that the treated cancer cells would not be replaced when they die, and hopefully the tumor would disappear.
"If it's possible to uncouple CPS from apoptosis, we can develop new drugs that would improve the effectiveness of treatments already in use," Shafikhani says.
In cancer cells, the CPS process and communication would need to be interrupted to prevent the development of new cancer cells; but in other conditions, the CPS process could be enhanced to accelerate the healing process. One of the possible long-term benefits of the discoveries set out in the new Developmental Cell article could be to use of these vesicles to encourage cell proliferation—in diabetic wounds where healing is not going well because tissue cells are dysfunctional and have reduced ability to regenerate, for example, Shafikhani says.















