July 6, 2017 report
Possible link found between eczema flare-ups and strain of bacteria
(Medical Xpress)—A team of researchers with the National Institutes of Health in the U.S. has found what appears to be a link between eczema flare-ups and a certain strain of bacteria. In their paper published in Science Translational Medicine, the group outlines their study of the connection between the skin ailment and bacteria and what they found.
Eczema is a skin condition causing patches of skin to become itchy and discolored. Besides being an irritant, it also causes emotional problems because most patients are young people, including children. Some studies have also shown it can lead to an increased likelihood of developing allergies. Prior research has suggested it might be possible that the condition is caused by some type of bacteria—some researchers have even found possible candidates. But despite evidence of higher numbers of certain bacteria existing on the skin during flare-ups, no one has been able to figure out if they were a cause or a side effect. In this new effort, the researchers sought to prove they were a likely cause.
The suspected bacteria, a strain of Staphylococcus aureus, lives on most people's skin, but because it appears to reproduce dramatically during flare-ups, the researchers sought a link. They enlisted the assistance of 18 volunteers, all children, and 11 of whom had eczema. The researchers scraped their skin to collect bacterial samples. For those with eczema, samples were collected during flare-ups, between flare-ups and just after flare-ups. Those without eczema only had their skin scraped once to offer as a comparison.
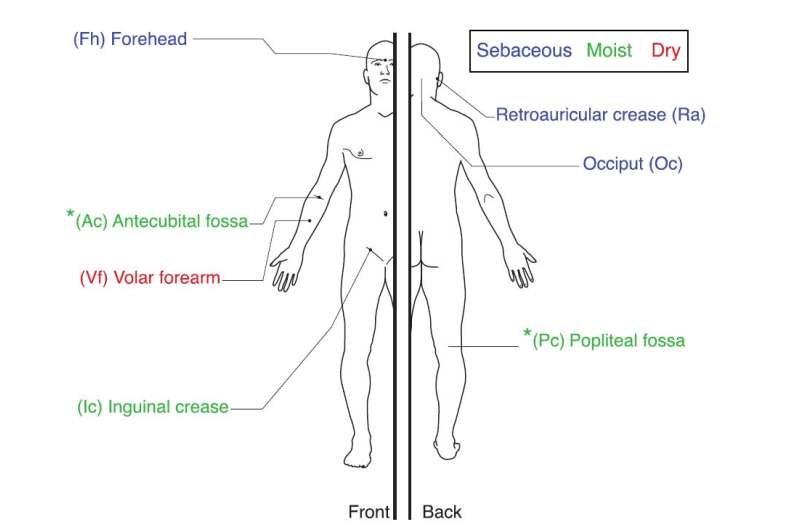
The researchers report that S. aureus was much more prevalent during flare-ups in the volunteers. They also noted that patients who experienced less severe flare-ups had more methicillin-resistant strains of the bacteria than did those who experienced more severe symptoms.
To find out if the bacteria was the cause of the flare-ups or merely a side effect, the researchers collected samples of the bacteria during a flare up and applied it to the skin of test mice. They report that doing so caused skin inflammation—much more so than when other strains of the same types of bacteria were applied.
The researchers acknowledge that their findings are not definitive proof that S. aureus causes eczema, but believe it indicates it is likely. More work needs to be done to determine why the bacteria suddenly multiply and to find out if there are other factors involved.
More information: Staphylococcus aureus and Staphylococcus epidermidis strain diversity underlying pediatric atopic dermatitis, Science Translational Medicine (2017). DOI: 10.1126/scitranslmed.aal4651 , stm.sciencemag.org/content/9/397/eaal4651
Abstract
The heterogeneous course, severity, and treatment responses among patients with atopic dermatitis (AD; eczema) highlight the complexity of this multifactorial disease. Prior studies have used traditional typing methods on cultivated isolates or sequenced a bacterial marker gene to study the skin microbial communities of AD patients. Shotgun metagenomic sequence analysis provides much greater resolution, elucidating multiple levels of microbial community assembly ranging from kingdom to species and strain-level diversification. We analyzed microbial temporal dynamics from a cohort of pediatric AD patients sampled throughout the disease course. Species-level investigation of AD flares showed greater Staphylococcus aureus predominance in patients with more severe disease and Staphylococcus epidermidis predominance in patients with less severe disease. At the strain level, metagenomic sequencing analyses demonstrated clonal S. aureus strains in more severe patients and heterogeneous S. epidermidis strain communities in all patients. To investigate strain-level biological effects of S. aureus, we topically colonized mice with human strains isolated from AD patients and controls. This cutaneous colonization model demonstrated S. aureus strain–specific differences in eliciting skin inflammation and immune signatures characteristic of AD patients. Specifically, S. aureus isolates from AD patients with more severe flares induced epidermal thickening and expansion of cutaneous T helper 2 (TH2) and TH17 cells. Integrating high-resolution sequencing, culturing, and animal models demonstrated how functional differences of staphylococcal strains may contribute to the complexity of AD disease.
© 2017 Medical Xpress



















