July 7, 2017 report
Existing malaria test found to be useful for predicting anemia risk from standard treatment
(Medical Xpress)—An international team of researchers has found that an existing kit for malaria testing can be used to identify patients at risk of developing anemia after receiving the standard treatment for the disease. In their paper published in the journal Science Translational Medicine, the group describes their study using the test to predict a serious form of anemia called post-artesunate delayed hemolysis (PADH) on malaria patients and how well it worked.
Malaria, as most are aware, is a condition in which a protozoan parasite invades the red blood cells and causes sickness. Worldwide, over three billion people live in regions where infections are prevalent. The modern treatment for the condition is to give patients a group of medications called artemisinins (drugs which contain an active compound found in the Artemisia plant), which work reasonably well. But after taking the drug, some patients (less than 5 percent) develop PADH several weeks later, which often leads to kidney failure. Unfortunately, until now, there has been no way to tell which people will develop PADH prior to treatment. In this new effort, the researchers report that they have found a test that offers some degree of accuracy in detecting the likelihood of malaria patients developing anemia after treatment.
The test is called the BinaxNOW malaria test kit, and is already used to test patients to see if they have malaria. Upon hearing anecdotal evidence of the test serving as a predictor of PADH, the researchers set up a study to find out if such claims were true. They administered the test to 95 Bangladeshi people along with 53 French visitors, all suffering from malaria, who also all received an artesunate. The researchers report that the test was 89 percent correct when looking for sensitivity and 73 percent for specificity.
As part of a separate study, the researchers also gave 49 patients quinine instead of artemisinins to treat their malaria. Quinine, though once used extensively, is no longer prescribed as a treatment for malaria because it has been found to cause other serious health problems. In their study, the researchers found that patients given quinine did not demonstrate high levels of a malaria protein called HRP2, which is what the BinaxNOW test measures to predict the likelihood of a patient developing PADH.

More information: Measuring the Plasmodium falciparum HRP2 protein in blood from artesunate-treated malaria patients predicts post-artesunate delayed hemolysis, Science Translational Medicine 05 Jul 2017: Vol. 9, Issue 397, eaaf9377 , DOI: 10.1126/scitranslmed.aaf9377
Abstract
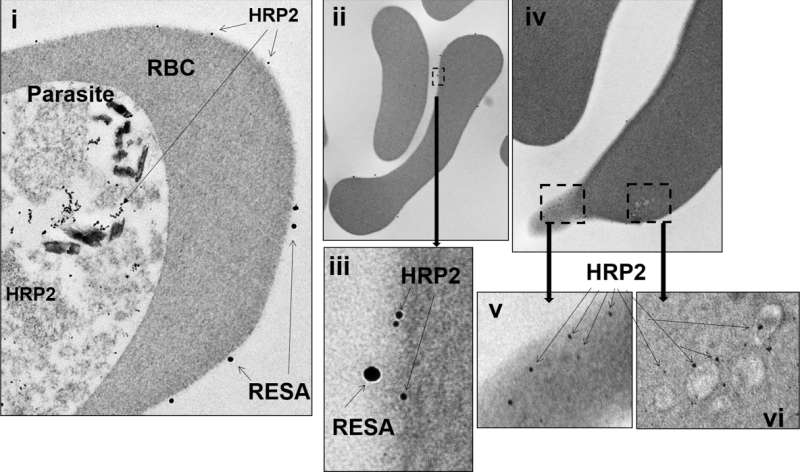
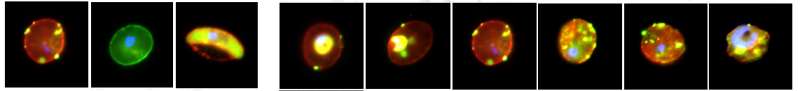
Artesunate, the recommended drug for severe malaria, rapidly clears the malaria parasite from infected patients but frequently induces anemia—called post-artesunate delayed hemolysis (PADH)—for which a simple predictive test is urgently needed. The underlying event in PADH is the expulsion of artesunate-exposed parasites from their host erythrocytes by pitting. We show that the histidine-rich protein 2 (HRP2) of the malaria parasite Plasmodium falciparum persists in the circulation of artesunate-treated malaria patients in Bangladesh and in French travelers who became infected with malaria in Africa. HRP2 persisted in whole blood (not plasma) of artesunate-treated patients with malaria at higher levels compared to quinine-treated patients. Using an optimized membrane permeabilization method, HRP2 was observed by immunofluorescence, Western blotting, and electron microscopy to persist in once-infected red blood cells from artesunate-treated malaria patients. HRP2 was deposited at the membrane of once-infected red blood cells in a pattern similar to that for ring erythrocyte surface antigen (RESA), a parasite invasion marker. On the basis of these observations, we developed a semiquantitative titration method using a widely available HRP2-based rapid diagnostic dipstick test. Positivity on this test using a 1:500 dilution of whole blood from artesunate-treated patients with malaria collected shortly after parasite clearance predicted subsequent PADH with 89% sensitivity and 73% specificity. These results suggest that adapting an existing HRP2-based rapid diagnostic dipstick test may enable prediction of PADH several days before it occurs in artesunate-treated patients with malaria.
© 2017 Medical Xpress



















