Why drugs don't reach cancer cells: Researchers develop technology to provide answers
For cancer patients, understanding the odds of a treatment's success can be bewildering.
The same drug, applied to the same type of cancer, might be fully successful for one person's tumour and do nothing for someone else. Physicians are often unable to explain why.
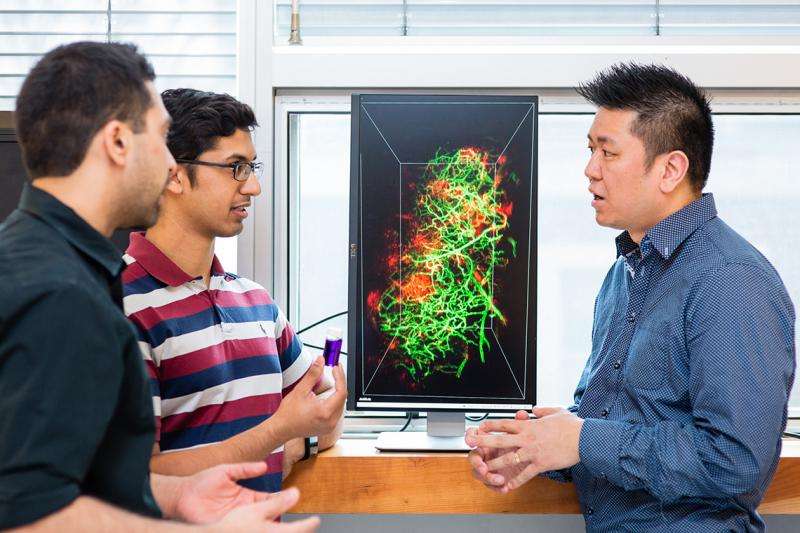
Now, University of Toronto researchers are beginning to understand one of the reasons. Biomedical engineering students Abdullah Syed and Shrey Sindhwani, and colleagues at the Institute of Biomaterials & Biomedical Engineering (IBBME), have created technology to watch nanoparticles entering into tumours – revealing barriers that prevent their delivery to targets and the variability between cancers.
"The biggest thing we've noticed is that nanoparticles face multiple challenges posed by the tumour itself on their way to cancer cells," says Sindhwani, an MD-PhD student working with Professor Warren Chan of IBBME. Syed and Sindhwani co-published their findings online and on the cover of the Journal of the American Chemical Society.
"So the treatment might work for a while – or worse, there's just enough of the drug for the cancer to develop resistance. This could be prevented if we can figure out the ways in which these barriers stop delivery and distribution of the drug throughout the cancer."
Tiny "nanoparticles" offer great hope for the treatment of cancer and other diseases because of their potential to deliver drugs to targeted areas in the body, allowing more precise treatments with fewer side-effects. But so far the technology hasn't lived up to its promise, due to delivery and penetration problems.
To dismantle this roadblock, the two graduate students searched for a way to better view the particle's journey inside tumours. They discovered that the tough-to-see particles could be illuminated by scattering light off their surfaces.
"The sensitivity of our imaging is about 1.4 millionfold higher," says Syed. "First, we make the tissue transparent, then we use the signal coming from the particles to locate them. We shine a light on the particles, and it scatters the light. We capture this scattering light to learn the precise location of the nanoparticles."
It was already understood that nanoparticles were failing to accumulate in tumours, thanks to a meta-analysis of the field done by researchers at U of T. But the researchers have developed technologies to look at nanoparticle distribution in 3-D, which provides a much fuller picture of how the particles are interacting with the rest of the tumour biology.
"The goal is to use this technology to gather knowledge for developing mathematical principles of nanoparticle distribution in cancer, similar to the way principles exist for understanding the function of the heart," says Syed.
And because each tumour is unique, this technology and knowledge base should help future scientists to understand the barriers to drug delivery on a personalized basis and to develop custom treatments.
The next step is to understand what, in cancer's biology, stops particles from fully penetrating tumours – and then to develop ways to bypass cancer's defences.
But the technology is also useful for diseases other than cancer. With the help of Professor Jennifer Gommerman, a multiple sclerorsis researcher in the department of immunology, Syed and Sindhwani captured 3-D images of lesions in a mouse model mimicking multiple sclerosis using nanoparticles.
"This is going to be very valuable to anyone trying to understand disease or the organ system more deeply," says Sindhwani.
Syed adds: "And once we understand barriers that don't allow drugs to reach their disease site, we can start knocking them down and improving patient health."
More information: Abdullah Muhammad Syed et al. Three-Dimensional Imaging of Transparent Tissues via Metal Nanoparticle Labeling, Journal of the American Chemical Society (2017). DOI: 10.1021/jacs.7b04022


















