Study adds to evidence that racial and economic factors affect surgical pain management
A "look back" analysis of more than 600 major colorectal surgeries using a "checklist" tool has added further evidence that racial and socioeconomic disparities may occur during many specific stages of surgical care, particularly in pain management.
A report of the study's findings by researchers at Johns Hopkins Medicine, published Sept. 11 in Diseases of the Colon & Rectum, documents the specific ways in which historically disadvantaged populations receive less optimal pain management and are placed on "enhanced recovery" protocols later than their wealthier and white counterparts.
"This study demonstrates that process measures, which guide and document each step of care, may be critical factors in preventing differences in care, particularly those due to race and socioeconomic status" says Ira Leeds, M.D., research fellow at the Johns Hopkins University School of Medicine and the paper's co-first author. "We can't fix what we don't measure," he adds.
Enhanced recovery after surgery (ERAS) protocols are predefined pathways designed to standardize some aspects of surgical care in order to reduce complications, decrease lengths of stay and improve overall patient satisfaction.
To determine whether ERAS had an impact, or revealed any racial and socioeconomic disparities after surgery, Leeds and colleagues performed a retrospective analysis of information gathered before and after the implementation of a colorectal ERAS pathway at The Johns Hopkins Hospital.
A total of 639 patient experiences (199 pre-ERAS implementation and 440 post-implementation) were used in the analysis, all surgeries performed between Jan. 1, 2013 and June 30, 2016. The research team collected socioeconomic information, medical diagnoses in addition to colorectal disease, and surgical outcomes information housed in Johns Hopkins' National Surgical Quality Improvement Program's internal database.
Data about participation in ERAS and adherence to process measures were obtained from the Johns Hopkins University School of Medicine's Department of Surgery quality improvement database.
Patients were categorized as either white or nonwhite patients, and low socioeconomic status or high socioeconomic status was determined by zip code. Some 75.2 percent of all patients were white and 91.7 percent were categorized as having a high socioeconomic status.
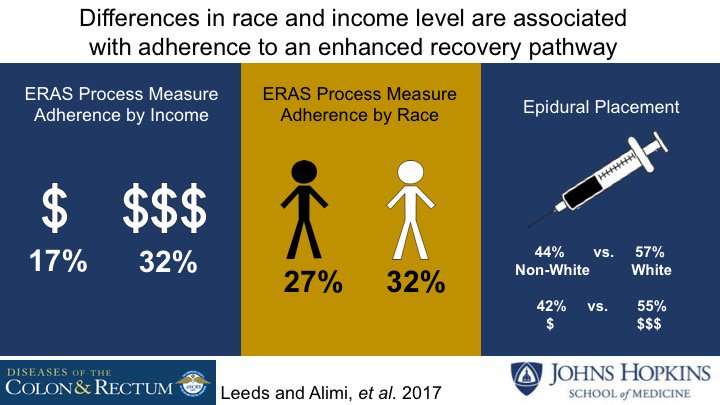
The researchers found that white patients were more likely to have transverse abdominis plane (TAP) blocks or epidurals initiated and maintained than nonwhite patients (57.1 versus 44.1 percent for initiation; 47.3 versus 34.3 percent for maintenance).
A similar trend for initiation of pain management was seen for high socioeconomic status patients (55.4 versus 41.5 percent). Leeds says this suggests that either nonwhite patients declined epidural blocks for pain management at higher rates due to inadequate counseling on the benefits, or that doctors carried implicit biases that led them to offer such pain management options less often to minorities and the poor.
Patients with a high socioeconomic status were placed on an ERAS pathway during scheduling more often than low socioeconomic status patients (69.7 versus 58.5 percent).
Prior to ERAS implementation, median lengths of stay, complication rates and total number of complications were not statistically different between white and nonwhite patients. Following ERAS implementation, median lengths of stay improved in both whites (a decrease of 1.5 days) and nonwhites (-1 days) and in patients with high socioeconomic status (-1 days) and low socioeconomic status (-2.0 days).
Following pathway implementation, the median lengths of stay improved in all subgroups with an overall decrease of 1 day, with no statistical difference by race or socioeconomic status. There were no significant differences in complication rates between racial (26.4 versus 28.8 percent) and socioeconomic groups (27.3 versus 25.0 percent) before ERAS implementation, and this was unchanged after ERAS implementation.
Leeds says the study results do not prove implicit racial or other bias as the cause of the differences in care, but they should, he says, heighten concern about the existence of such disparities and renew attention toward identifying and addressing bias.
While Leeds acknowledges the study's limitations of only including one institution and drawing from two datasets not designed to be merged for analysis, he notes that the findings add evidence regarding the efficacy of ERAS pathways in identifying disparities and highlight how short-term disparities can be mitigated by quality monitoring.
Two of the co-authors on this paper, Elizabeth Wick, M.D., and Deborah Hobson from Johns Hopkins, are currently leading efforts to enable more than 750 hospitals across the U.S. to implement ERAS.
More information: Ira L. Leeds et al. Racial and Socioeconomic Differences Manifest in Process Measure Adherence for Enhanced Recovery After Surgery Pathway, Diseases of the Colon & Rectum (2017). DOI: 10.1097/DCR.0000000000000879


















