Four reasons that could explain ACOs' sluggish savings
Despite aggressive targets set by the Medicare for the spread of value-based payment arrangements, such as accountable care organizations, achieving lower spending growth has proved extremely challenging. In an article in the November issue of the New England Journal of Medicine, Dartmouth Institute Professors Valerie Lewis, Elliott Fisher, and Carrie Colla offer four explanations—two economic and two organizational—as to why the nearly 1,000 organizations operating as ACOs have generated limited savings. As the authors note, even in the third year of Medicare ACO contracts, fewer than half of ACOs received a bonus for reduced savings.
Through the lens of diversity:
Medicare sets few constraints on the forms ACOs can take, and they are remarkably diverse—including both longstanding integrated health systems and relatively recently formed entities, such as hospitals and private physician practices that have come together to pursue ACO contracts.
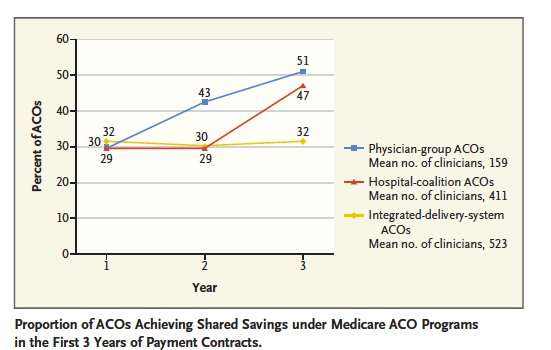
In order to understand the performance of ACOs in context of such diversity, The Dartmouth Institute team paired data from the Centers for Medicare and Medicaid Services and the National Survey of ACOs to compare performance in the first three years of ACO contracts for three types of ACOs: integrated delivery systems, out-patient-physician-practice ACOs and coalitions of independent hospitals and practices. In the first year of ACO contracts, approximately 30% of ACOs in each group received bonuses. After that, the trends differ: The percentage of integrated delivery systems receiving bonuses remaining constant, while among hospital coalitions that 30% figure held steady in year two but jumped to 47% in year three. Meanwhile, the percentage of physician-group ACOs achieving savings increased steadily to 43% in year two and 51% in year three.
Economic and Organizational Barriers
The authors then identified four cross-cutting reasons for the failure of ACOs to achieve savings:
- Weak incentives/no downside risk (economic): Nearly all participants in the Medicare Shared Savings program, receive a bonus if they generate savings but bear no financial responsibility for losses. It's possible sharing in downside risk could result in greater behavior changes among providers and, as a result, greater savings.
- Not enough patients covered by ACO-like contracts (economic): The authors note that until providers reach a tipping point in the number of patients covered by ACO-like contracts, it will be hard for organizations to generate substantial savings, as initiatives that generate savings in the care of a provider's ACO patients will reduce income from its fee-for-service patients.
- Knowledge development: Outpatient-physician-practice ACOs and some newer hospital-coalition ACOs in particular may need time to explore care management models or learn how to improve care transitions.
- Complexity/laying a foundation: Most ACOs are not pre-existing organizations but a collection of independent providers. These ACOs have to do a great deal of foundational work to set up a functional ACO so progress toward generating savings may be delayed as a result. (*The authors note that institutional complexity probably affects integrated organizations as well as "overcoming inertia in these systems may be like trying to turn a large battleship."
In light of the diversity of ACOs, the authors recommend a flexible approach to motivating and rewarding providers.
"The ACO experiment has yielded results that are underwhelming to date," said lead author Valerie Lewis, PhD. "In thinking through refinements or redesign, policymakers should give careful consideration to the diversity of ACOs. The balance of pushing hard enough with incentives while also allowing time for ACOs to grow and develop is tricky, but getting this right could ultimately lead to more successful programs—and greater savings."
More information: New England Journal of Medicine (2017). DOI: 10.1056/NEJMp1709197












