Device enhances radiation therapies
For many cancer patients, going through radiation therapy can be an incredibly stressful and time-consuming process. Dalhousie's Dr. James Robar wants to change that by providing health practitioners with an in-house tool that improves the accuracy and efficiency of this treatment, while making it a more comfortable experience for the patient.
Radiation oncologists and medical physicists have access to high tech equipment, state-of-the-art software and linear accelerators to deliver treatment in a highly automated way, but there are key steps of the process that remain very manual. These include using a device called a bolus, which is a layer of tissue-equivalent material placed on the patient's skin during treatment that assists in providing the optimal dose of radiation.
Currently, the bolus is generally made out of a rubbery material called SuperFlab. Although this has been the industry standard for decades, it does have some drawbacks.
"The SuperFlab doesn't always conform to the surface very well," says Dr. Robar, who is a professor in the Faculty of Medicine. "This may cause air gaps, which inadvertently decreases the dose of radiation to the surface."
To get around this, radiation therapists often have to use decidedly lower tech materials like wax, linens and tape to make it fit as well as possible.
"If you tour a clinic like this, you'll see rooms that look like arts and crafts studios, where radiation therapists are trying to be sculptors essentially and build things for the patients," says Dr. Robar. "There are a few consequences of that approach. It has limited accuracy in many cases, and can take a lot of time. It's not only a time-sink for the patient, but also for the radiation therapists and other staff."
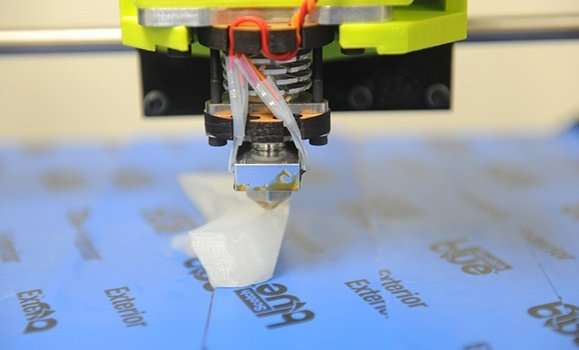
Dr. Robar was determined to find a better way, and with 3-D printing becoming increasingly more accessible, he saw an opportunity, starting in 2012. By using existing CT images that are acquired for patients as a part of standard procedure and a 3-D printer, he figured that he could create devices for that were tailored to fit each specific patient accurately.
Enhancing the accuracy and efficiency of radiation therapy
With a Proof-Of-Concept (POC) grant from Springboard Atlantic, Dr. Robar and his team purchased their first 3-D printer, and began creating four different devices.
Electron Beam Therapy
The linear accelerator also produces electron beams, which are used to treat tumours closer to the surface of the patient. Dr. Robar's team developed novel algorithms that produce a 3-D printed bolus that will modulate the energy of the electron beam, tailoring the treatment to the patient.
"For this application, we need to produce a dose distribution that conforms to the tumor, by varying the depth of the bolus over the tumour, depending on the depth of the tumour below the surface," says Dr. Robar. "As a result, we produce a dose distribution that matches the shape of the tumor, and much of the healthy tissue is spared."
This was the very first 3-D printed device that Dr. Robar's team created. One of his students in the Dal Medical Physics Graduate Program, Shiqin Su, was responsible for developing the algorithm.
Photon Beam Therapy
"It was quite a natural initial idea to try to produce some highly automated software that produces photon bolus, says Dr. Robar. "Our task was to design a bolus and fabricate it, so that it fits the patient and provides the required dose build-up for treatment."
The x-ray photons used in radiation therapy are approximately 100 times more energetic than x-rays used in imaging, and are designed to kill cancer cells. One application of 3-D printed photon bolus is used during treatment of the chest wall for patients who have received mastectomy. An adequate radiation dose must be delivered to the surface of the chest wall, and Dr. Robar's team has recently completed an in-house study to evaluate the new technology for that indication.

"One of my favorite uses of photon bolus was for a patient who had a tumor on his nasal septum," says Dr. Robar. "He had undergone surgery but the tumor recurred, so we wanted to treat him using photon radiotherapy. The patient hadn't been to our clinic before but he had a previous CT imaging for diagnoses and follow-up with his surgery."
With that information, Dr. Robar was able to look through the image archival system, and pull his CT scan to design a bolus which fit perfectly in his nose before he even stepped foot in the clinic.
"We put topical anesthetic on it, and it fit his nose perfectly." says Dr. Robar, "We could verify that because he had to have a CT scan that day. It worked really well. He had 30 treatments with this device and by the end of his treatment course, he would hop on the treatment bed, grab his 3-D printed nose bolus, insert it himself, snap it together and he was ready to go."
Immobilization Device
The next application is an immobilization device, which was specifically designed for breast cancer treatment for an intact breast. Usually, this treatment is administered over 16 to 25 weekdays in a row. Breasts are highly mobile, which can cause an inconsistent dose of radiation to be delivered over this period of time.
The idea was to create a bolus that would act like a shell, and use a highly stiff version of 3-D printing materials to keep the breast in place. The capacity to create a complex but hollow structure that is tailored to the patient is a unique feature of 3-D printing, and by using this technology to minimize the amount of material in the path of the beam, it limits the skin dose and the associated severe toxicity.
Brachy therapy
Brachy therapy treats tumors on both the inside and the surface of the patients by delivering radiation to the tumor through a radioactive source.
Currently, an accessory called the "Freiburg flap" is used for treating tumours near the surface of the patient. It consists of a beaded sheet that must be manually affixed to the patient, for example, by sewing to a mask or cast. Catheters pass through these beads, which allows the application of a radioactive source to treat a tumour on the patient.
The downfall of the Freiburg flap is that practitioners have to try and force the blanket of beads to conform to the anatomy.
This is not an easy task, and Dr. Mammo Yewondwossen, also on the Medical Physics team, thought that this process could be improved by 3-D printing a custom applicator. Another Dal Medical Physics Graduate Student student, Scott Clarke, helped develop the technology for this particular device.
All of these applications have been shown to greatly enhance the accuracy and efficiency of the radiation treatment process. The next step is to put it in the hands of clinicians.
The 3-D printing technology was licensed over 18 months ago from Dalhousie's Industry Liaison and Innovation, and from there a start-up company called 3-D Bolus was formed to begin developing the product. The product includes the software that will enable practitioners to create photon and electron boluses, low-density immobilization and brachytherapy surface applicators. The application is bundled with a 3-D printer.
"The team has gone to multiple industry trade shows, including big ones that are part of conferences every year in the states, Canada, Europe, and there's been a resounding response to this technology," says Dr. Robar. "It's been really enjoyable for me to watch because I get to walk by the trade show booth and witness all the interest in 3-D Bolus' software."
Currently version one of the product has been developed and has secured CE Mark clearance. The technology has been deployed in clinics in Dublin, Ireland and Tel-Aviv, with research versions in Chicago, San Francisco and Halifax.
"The hope is for this to become the standard model of treatment. In order to achieve that, we have to make this as practical and reliable as possible, otherwise we're not going to meet that goal," says Dr. Robar. "Delivery of radiotherapy involves extremely busy clinicians who need to use these tools, and they can't resemble a research project. It has to be an entirely turn-key solution. It's getting very close to being at that point."
Going forward, the company's approach will be to bring in 10 founding clients who will be the first in the world to use the technology in the clinic and to assist with testing and further development. Once they receive Food and Drug Association (FDA) clearance, slated for early 2018, they will begin sales in the US.

















