Gastric bypass and sleeve gastrectomy are comparable for morbid obesity treatment
In Switzerland, 5,500 operations to combat morbid obesity are conducted every year. Gastric bypasses and sleeve gastrectomy operations perform similarly: patients lose two-thirds of their excess weight in the long term, as researchers from the University of Basel at the St. Claraspital report in the Journal of the American Medical Association (JAMA). When it comes to gastric acid reflux, the bypass clearly shows better results.
Morbid obesity and associated diseases such as diabetes, cardiovascular diseases and cancer are widespread in the western world. Surgical interventions are currently considered to be the most effective measure in severely obese people with a BMI over 35.
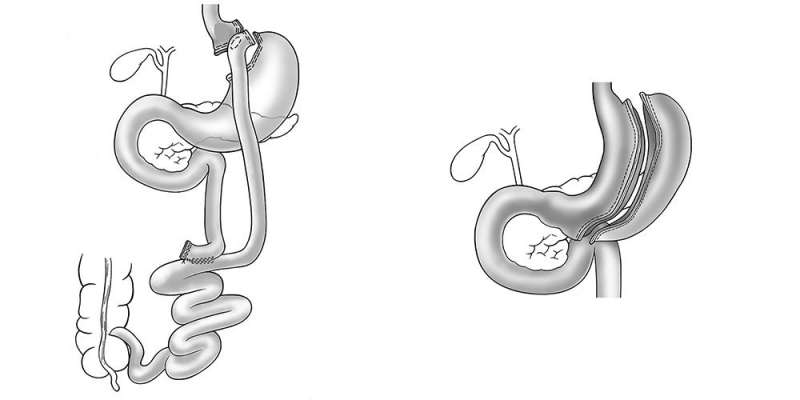
The standard surgery is a gastric bypass, where part of the stomach and small intestine is bypassed. Other methods are also becoming more popular, such as sleeve gastrectomy, in which the volume of the stomach is reduced. This operation is technically easier to perform and can be done with low complication rate even in patients with very high BMI.
More than 200 patients examined
To compare these two common types of surgery, the study looked at 217 morbidly obese patients; half were assigned to a gastric bypass and half a sleeve gastrectomy. Their average age was 45.5 years, and 72 percent of them were women. The study was conducted at four locations in Switzerland and was led by Professor Ralph Peterli from the University of Basel at St. Claraspital.
In terms of weight loss, the two types of surgery led to similar results five years after the surgery: the patients lost 68 percent of their excess weight after a gastric bypass, and 61 percent after a sleeve gastrectomy. The BMI also fell from 44 to 32 after both operations. Associated diseases such as hypertension, diabetes, altered blood lipids, back/joint pain and depression were also improved, as well as general quality of life.
Improvement in gastric acid reflux
Patients with existing gastric acid reflux benefited more from a gastric bypass operation: after this procedure, symptoms were eliminated in 60 percent, compared to only 25 percent after a sleeve gastrectomy. Sleeve gastrectomy also led to a deterioration or new onset of gastric acid reflux significantly more often. Further surgery or interventions were needed in 22 percent of gastric bypasses and 16 percent of sleeve gastrectomy operations.
More information: Ralph Peterli et al. Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss in Patients With Morbid Obesity, JAMA (2018). DOI: 10.1001/jama.2017.20897


















