Malnutrition frequently underdiagnosed and undertreated among hospital patients
Malnutrition among hospitalized patients remains a serious issue that has been underdiagnosed and undertreated for decades. It is estimated that nearly one out of five pediatric patients and one out of three adult patients aged 60 and older are malnourished. In the current issue of the Journal of the Academy of Nutrition and Dietetics healthcare experts focus on the latest findings in hospitalized patients with malnutrition in the US and present data elucidating the extent of this serious healthcare issue.
Harvard surgeon Charles Butterworth, Jr., MD, acknowledged the severity of malnutrition among hospitalized patients in 1974 in his landmark article, "The Skeleton in the Hospital Closet." Since that time, multiple studies have shown direct associations between malnutrition and higher rates of hospital length of stay, complications, readmission, and mortality. Malnutrition is a major contributor to multiple morbidities, decreased physical and cognitive function, and impaired quality of life, as well as increased hospital readmissions and overall higher healthcare costs. A 2012 consensus statement from the Academy of Nutrition and Dietetics and the American Society of Parenteral and Enteral Nutrition (ASPEN) has led efforts to improve the recognition, diagnosis, and treatment of malnutrition in hospital settings. The consensus statement defined the current standard of care for assessing malnutrition based on the presence of at least two of the following clinical characteristics: insufficient energy intake, weight loss, loss of muscle mass, loss of subcutaneous fat, localized or general fluid accumulation, and diminished grip strength.
In one of the largest studies of its kind, researchers at the University of Iowa evaluated close to six million adult hospitalizations at 105 institutions during 2014-2015 using a large collaborative multi-institutional database to assess the rate of malnutrition diagnoses and institutional variables associated with higher rates of malnutrition diagnosis. They determined that only 5% of hospitalized adult patients had medical diagnoses of malnutrition during their hospital stay. This rate was consistently low across different hospitals. The researchers found that institutional culture influences missing malnutrition diagnoses. Hospitals with higher rates of malnutrition identification had a higher volume of patients, higher hospital ranking, and greater patient satisfaction.
"The value of establishing a malnutrition diagnosis is to prompt malnutrition-based interventions because malnutrition represents a potentially modifiable risk factor in patient care," explains Kenneth G. Nepple, MD, FACS, Associate Professor of Urology in the Department of Urology and Holden Comprehensive Cancer Care Center at the University of Iowa, who led the study. "Real-world data identified an alarmingly low rate of malnutrition diagnoses in comparison to prior focused research efforts, which suggests failure to identify at-risk patients. Quality improvement efforts aimed at enhanced structure and process appear to be needed to improve the identification of malnutrition."
Maria Isabel Toulson Davisson Correia, MD, PhD, of the Universidade Federal de Minas Gerais, Belo, Brazil, welcomes the study led by Dr. Nepple. In an accompanying editorial she comments that "the phenomenon of missing malnutrition diagnoses across academic centers is an alarming reality. Nutrition diagnosis is a first step to providing adequate overall nutrition medical therapy. The authors have touched on a sensitive issue that demonstrates the influence of an institution's culture. This suggests that quality improvement efforts aimed at a better structure and process have a key role in improving the identification of malnutrition and, perhaps, the overall nutrition care pathway. Teamwork is fundamental!"
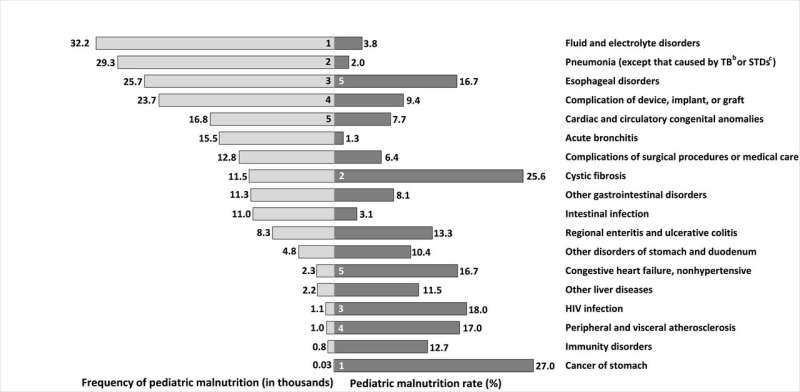
Pediatric malnutrition is also underdiagnosed according to a team of clinicians and epidemiologists who analyzed 10 years of data from a nationally representative database of pediatric inpatient hospitalizations in the US to describe the prevalence, trends, and short-term outcomes of children receiving a coded diagnosis of malnutrition. Of the 2.1 million pediatric patients hospitalized annually, more than 54,600 had coded diagnoses of malnutrition (2.6%). The prevalence increased from 1.9% in 2002 to 3.7% in 2011. Children with malnutrition experienced worse clinical outcomes, longer lengths of stay, and increased costs of inpatient care. Highest rates were among patients with stomach cancer, cystic fibrosis, and human immunodeficiency virus.
"Pediatric malnutrition in inpatient settings is currently underdiagnosed, which disproportionately impacts children with special healthcare needs, vulnerable populations, and underserved facilities. With improved recognition and proper diagnosis, those most in need are more likely to receive timely intervention which would prevent further clinical decline and improve long-term outcomes for patients," says lead investigator Jenni Carvalho-Salemi, MPH, RDN, LD, CNSC, of the Department of Renal and Pheresis Services, Department of Food and Nutrition Services, Texas Children's Hospital, Houston, TX.
The study points to discrepancies in coding, which highlight the need for improved nutrition education and awareness among healthcare providers, as well as the integration of registered dietitian nutritionists into multi-disciplinary acute care teams. According to Ms. Carvalho-Salemi, "Our findings underscore the need for a nationwide benchmarking program for early identification of at-risk patients. Accurate documentation is not only necessary to provide quality care, but also for appropriate hospital- and provider- reimbursement and adequate resource allocation."
Physicians at the Erasmus Medical Center, Sophia Children's Hospital, Rotterdam, The Netherlands, highlight the far higher rates of malnutrition among hospital patients reported in other developed countries. In these studies, a prevalence of between 6.1% and 11.9% was found for acute malnutrition (based on weight), between 7.2% and 10% for chronic malnutrition (based on height), and between 13.3% to 20% for overall malnutrition.
"The US study showed pediatric malnutrition to be associated with higher infection rates, unlike a recently published large prospective study among 14 tertiary hospitals in 12 countries in Europe, in which 2,567 children were assessed upon admission," comment Jessie M. Hulst, MD, PhD, pediatric gastroenterologist, and Koen F.M. Joosten, MD, PhD, pediatric intensive care physician. "While malnourished children in the European study had a longer length of stay and more diarrhea and vomiting than children in good nutritional status, there were no associations with infections."
Malnutrition is present in 30% to 50% of hospitalized patients aged 60 or older, according to research led by Heidi J. Silver, PhD, MS, RDN, associate professor at the Vanderbilt Center for Human Nutrition at Vanderbilt University Medical Center, Nashville, TN. In contrast, only 11% of patients had a malnutrition diagnosis documented in the electronic health record by medical providers.
The Vanderbilt team conducted a pilot intervention to evaluate the Malnutrition Quality Improvement Initiative (MQii). This three-month intervention aimed to reduce the burden of hospital malnutrition by training and educating healthcare providers to improve screening, assessment, diagnosis, and treatment for malnutrition. Participants were 45 healthcare professionals from geriatric, general medicine, and general surgery units at Vanderbilt University Hospital.
This intervention significantly improved the malnutrition knowledge of the enrolled healthcare providers. It also increased the number of older patients diagnosed and treated for malnutrition as well as the number of patients whose malnutrition care was continued beyond the hospital stay into their discharge plan.
"Malnutrition in older adults most often goes unidentified, undiagnosed, and untreated. This is partly due to the lack of training and education of healthcare providers in the clinical characteristics of malnutrition in today's adults, who may be overweight or obese but also malnourished," explained Dr. Silver. "Unfortunately, in today's adults, being overweight or obese masks the presence of malnutrition. It is important to understand that malnutrition contributes to immune system compromise, infections, poor wound healing and development of pressure sores, physical frailty, and falls and fractures. The gaps in diagnosis and treatment of malnutrition also affect older adults by promoting longer hospital stays, more ICU admissions and hospital readmissions, and admission to assisted living and nursing homes. By improving malnutrition knowledge, diagnosis, intervention, and the timeliness of these activities, we can prevent the serious consequences and burden of malnutrition on patients, caregivers, and our healthcare system."
More information: Conrad M. Tobert et al, Malnutrition Diagnosis during Adult Inpatient Hospitalizations: Analysis of a Multi-Institutional Collaborative Database of Academic Medical Centers, Journal of the Academy of Nutrition and Dietetics (2017). DOI: 10.1016/j.jand.2016.12.019

















