Could viruses take cancer immunotherapy to the next level?
Immunotherapy, which helps the body's immune system attack cancer, has revolutionized treatment for cancers such as melanoma and leukemia. However, many other kinds of cancer remain resistant. A new study led by researchers at The Ottawa Hospital and the University of Ottawa suggests that a combination of two immunotherapies (oncolytic viruses and checkpoint inhibitors) could be much more successful in treating breast cancer and possibly other cancers. Their study, which uses mouse models, is published in Science Translational Medicine.
"It was absolutely amazing to see that we could cure cancer in most of our mice, even in models that are normally very resistant to immunotherapy," said Dr. Marie-Claude Bourgeois-Daigneault, lead author of the study and a postdoctoral fellow in Dr. John Bell's group at The Ottawa Hospital and the University of Ottawa. "We believe that the same mechanisms are at work in human cancers, but further research is needed to test this kind of therapy in humans."
In the current study, the researchers focused on "triple negative" breast cancer, which is the most aggressive and difficult-to-treat kind of breast cancer.
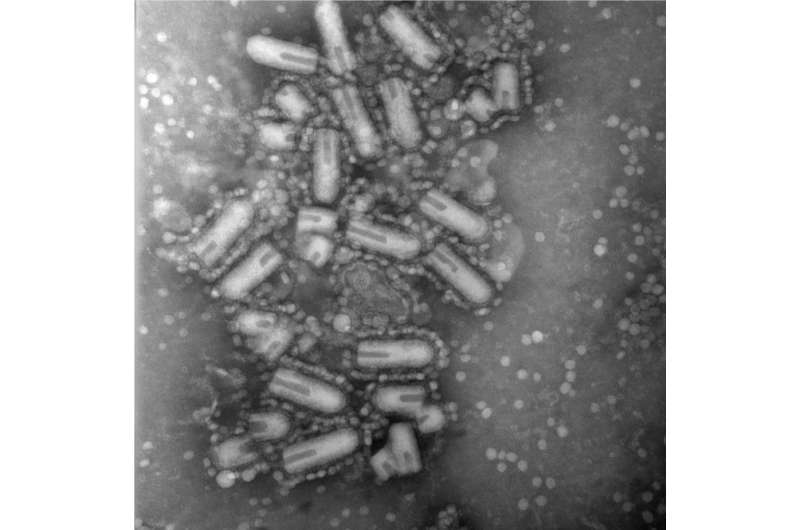
The researchers studied three mouse models of triple negative breast cancer, and found that all were resistant to a checkpoint inhibitor which is commonly used to treat other kinds of cancer. They also found that while an oncolytic virus called Maraba could replicate inside these cancers and help the mouse's immune system recognize and attack the cancer, the virus alone had minimal impact on overall survival.
The researchers then tested the virus and checkpoint inhibitor together in models that mimic the metastatic spread of breast cancer after surgery, which is very common in patients. They found that this combination cured 60 to 90 percent of the mice, compared to zero for the checkpoint inhibitor alone and 20 to 30 percent for the virus alone. In these models, the virus was given before the surgery and the checkpoint inhibitor was given after.
"Our immune system is constantly trying to recognize and kill cancer cells, but the cancer cells are always trying to hide from it," explained Dr. Bell, senior scientist at The Ottawa Hospital and professor at the University of Ottawa. "When you infect a cancer cell with a virus, it raises a big red flag, which helps the immune system recognize and attack the cancer. But in some kinds of cancer this still isn't enough. We found that when you add a checkpoint inhibitor after the virus, this releases all the alarms and the immune system sends in the full army against the cancer."
A recently-published clinical trial confirmed that oncolytic viruses and checkpoint inhibitors have potential for treating melanoma, but this is the first study to show the potential in breast cancer. It is also the first study to test viruses and checkpoint inhibitors in a surgery and metastasis model, which is particularly relevant for patients.
More information: M.C. Bourgeois-Daigneault el al., "Neoadjuvant oncolytic virotherapy before surgery sensitizes triple-negative breast cancer to immune checkpoint therapy," Science Translational Medicine (2017). stm.sciencemag.org/lookup/doi/ … scitranslmed.aao1641
Related: A. Samson el al., "Intravenous delivery of oncolytic reovirus to brain tumor patients immunologically primes for subsequent checkpoint blockade," Science Translational Medicine (2017). stm.sciencemag.org/lookup/doi/ … scitranslmed.aam7577


















