A blueprint for future blood-nerve barrier and peripheral nerve disease research
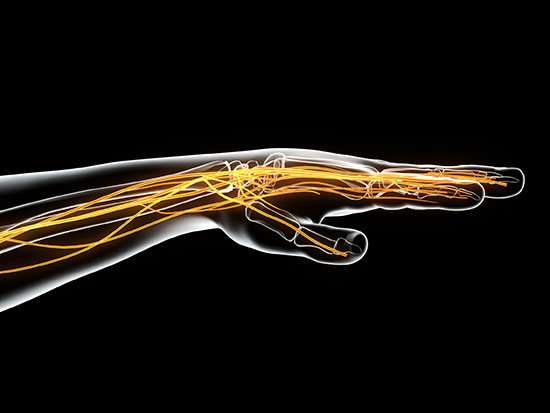
Human peripheral nerves—all the nerves outside of the central nervous system—are protected by the blood-nerve barrier. This is a tight covering of endothelial cells that maintains the microenvironment within the nerves by restricting the amounts or types of water, ions, solutes and nutrients that can reach the axons, or electric cables within the nerves, from the blood circulation system.
This allows the nerves to function.
"I describe these endothelial cells as a gate or door that controls what goes into and out of the nerve; it is the gateway between the systemic blood circulation and the peripheral nerves," said Eroboghene Ubogu, M.D., professor of neurology at the University of Alabama at Birmingham.
Little is known about the components that make up this door, and without that knowledge, neurologists like Ubogu are hard-pressed to develop specific treatments for the 20 million to 30 million U.S. patients, and hundreds of millions worldwide, with peripheral nerve disease. "If we don't understand what makes up this door that allows materials to go in or out, and how the door really works, how can we come up with specific treatments when nerves do not work?" Ubogu said.
In research published in Scientific Reports, Ubogu and UAB colleagues—for the first time—describe the transcriptome of these specialized cells called endoneurial endothelial cells, finding 12,881 RNA transcripts that define the normal human blood-nerve barrier. These messenger RNAs are the templates for a cell's building blocks, the proteins that provide structure and function to the living cell.
Previous research on the blood-nerve barrier tended to look at just one or a few cell components at a time. The transcriptome reveals every component active in normal endoneurial endothelial cells that form the human blood-nerve barrier.
"It is as if previously we worked before with a little flashlight," said Ubogu, who has studied the blood-nerve barrier since 2007. "This is a huge, revealing floodlight. For example, I probably knew no more than six components of the tight junctions present at the blood-nerve barrier. With this paper, we came up with 133 components involved in tight and adherens junctions. This is like a dream come true."
Knowledge of normal RNA and protein expression in the endoneurial endothelial cells provides an essential blueprint or reference guide. This guide will help physicians and researchers understand how peripheral nerves are kept healthy and help clinicians and medical chemists figure out which transporters are active in endoneurial endothelial cells, so they can design drug treatments that can actually reach the nerves or are prevented from causing toxic damage to nerves. The guide can also direct translational research in peripheral neuropathies by observing how components may be disrupted or altered during disease or injury, and help develop better treatments for chronic pain.
Ubogu's study started from normal frozen human sural nerves preserved in the Shin J. Oh Muscle and Nerve Histopathology Laboratory at UAB. The sural nerve, found in the outer calf region of the leg, is commonly biopsied as part of certain peripheral neuropathy workups.
The UAB team isolated RNA transcripts from the blood-nerve barrier forming microvessels directly from the frozen sural nerve tissue using a specialized technique called laser-capture microdissection. At least 200 microvessels were collected from two female and two male adults who had normal nerve biopsies. The team also isolated RNA from purified endoneurial endothelial cells previously isolated from an adult woman and grown in tissue culture. They isolated RNA from three passages, or early, and eight passages, or late, for this study. The early and late comparison was to make sure the RNA did not change in these cells because of tissue culture.
RNA from the endoneurial microvessels and endothelial cells was sequenced. For the microvessels from the biopsies, called the in situ blood-nerve barrier, transcripts had to agree for at least three of the four sources. For the endoneurial endothelial cells from tissue culture, called in vitro blood-nerve barrier, transcripts had to agree at both passages. The researchers found 12,881 RNA transcripts that were common to the in situ and in vitro blood-nerve barrier. The tissue-cultured endoneurial endothelial cells acted as a control to correct for possible contamination of the in situ blood-nerve barrier by cells like pericytes and leukocytes present with microvessels during laser-capture microdissection.
The transcriptome was validated two ways. First, the transcriptome was found to include previously identified vascular endothelial markers, enzymes, scavenger receptors, mitogen receptors, nutrient transporters, cellular adhesion molecules, chemokines, adherens and tight junction, and junction associated molecules. Second, the researchers showed expression, as detected by indirect fluorescent immunohistochemistry, of specific proteins that were identified by this study in the sural nerve endoneurial microvessels of another adult woman with a normal biopsy. This included markers that had and had not been previously identified in these endothelial cells—31 selected cell membrane, chemokine receptor, cytoskeletal, junctional complex and secreted proteins.
Ubogu expects a host of translational work to build upon this research.
Knowledge of the components and regulators of small molecule and macromolecular transport unique to the human blood-nerve barrier can aid development of drugs that can use the array of influx transporters, channels and receptor-mediated transcytosis components to reach the nerves. This is important in developing effective drugs for peripheral neuropathies and treating chronic neuropathic pain, a condition that affects 1 percent to 10 percent of people worldwide. This is crucially important as the world deals with the opioid crisis and seeks better treatments, with fewer side effects, for chronic pain.
Knowing the molecules relevant for growth of blood vessels and formation of intercellular junction complexes could guide therapeutic strategies to repair peripheral nerves after traumatic injury. This knowledge could also help restore and preserve peripheral nerve function in patients with peripheral neuropathies from other reasons, such as diabetes and cancer.
Ubogu says the study provides essential information on the possible determinants of leukocyte trafficking during normal immunosurveillance and the biological networks that may be involved in peripheral nerve innate and adaptive immune responses. This could improve our understanding of how the human blood-nerve barrier responds to injury, viral infections or microbial entry from the bloodstream into peripheral nerves.
The work could also help us better understand the pathogenesis and targeted treatment of peripheral nerve-restricted autoimmune disorders such as Guillain-Barré syndrome and chronic inflammatory demyelinating polyradiculoneuropathy, two conditions that can lead to loss of productivity and economic independence, chronic pain or disability.
"The unique resources within the UAB neuromuscular division and the collaboration with the UAB Heflin Center for Genomic Science were essential to this project to figure out the human blood-nerve barrier transcriptome as quickly and comprehensively as we did," Ubogu said.
More information: Steven P. Palladino et al, The Human Blood-Nerve Barrier Transcriptome, Scientific Reports (2017). DOI: 10.1038/s41598-017-17475-y













