Confronting TB resistance
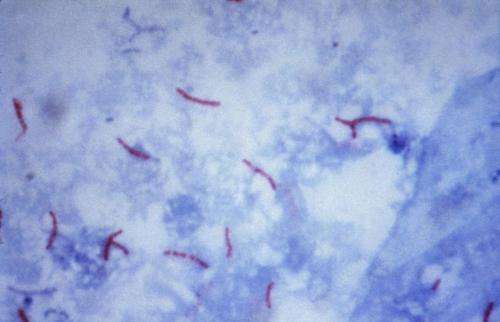
Tuberculosis, caused by Mycobacterium tuberculosis, is a highly infectious lung disease in humans.Unfortunately, resistance to anti-tubercular medicines such as fourth-generation fluoroquinolones is on the rise. In most cases, fluoroquinolone resistance is caused by mutations in a bacterial enzyme called gyrase.
Compounds called M. tuberculosis gyrase inhibitors (MGIs) display activity against tuberculosis in cellular and animal models, but little is known of their interaction with the bacterial enzyme.
Neil Osheroff, Ph.D., and colleagues examined the mechanism of action of MGIs against purifiedM. tuberculosis gyrase. They report that MGIs effectively increase levels of gyrase-mediated single-stranded DNA breaks, which lead to chromosomal fragmentation, and maintain activity against commonly mutated fluoroquinolone-resistant forms of the enzyme.
This mechanistic study, reported in the journal ACS Infectious Diseases, provides an important insight into anti-tubercular drug activity. Furthermore, it highlights the use of MGIs as potent anti-tubercular medicines and their potential in overcoming the serious threat of multi-drug resistant tuberculosis.
More information: Elizabeth G. Gibson et al. Mechanism of Action of Mycobacterium tuberculosis Gyrase Inhibitors: A Novel Class of Gyrase Poisons, ACS Infectious Diseases (2018). DOI: 10.1021/acsinfecdis.8b00035


















