New hepatitis C drugs mean diseased organs can be used for transplants
Unthinkable until a few years ago, the practice of putting hepatitis C-infected organs into uninfected patients has been embraced by the transplant world as a way to whittle long waiting lists for life-saving kidneys, livers, hearts and lungs.
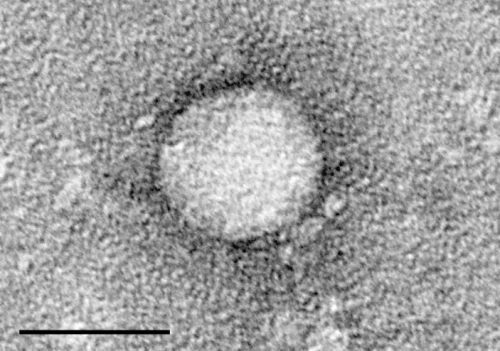
The main reason for this about-face is simple: New, easy-to-tolerate antiviral drugs with better than 95 percent effectiveness have transformed the treatment of hepatitis C, a virus that can slowly destroy the liver. A small but growing body of research by the University of Pennsylvania and other pioneers shows these medications can cure hep C infection in transplant patients who accept infected organs, typically with just four to 12 weeks of therapy. At the same time, the opioid crisis has meant there are more organs available from people with hep C, which can be spread by the use of injection drugs.
Now, the question is whether this approach should continue to be studied in clinical trials, or opened right away to the 114,000 Americans awaiting transplants. Patients are told about the potential risks of accepting organs with the virus and do not lose their place on transplant lists if they decline.
At least one transplant center, at the University of Washington, is not holding off. It announced in June that all heart transplant patients will be offered suitable hearts from hep C-infected donors. Infected hearts may eventually account for as many as eight of the 48 heart transplants UW performs annually, it said in a press release.
"Greater donor-organ availability means faster transplants for people on the wait list—and shorter waits are associated with better patient outcomes," said Shin Lin, a UW cardiologist and heart transplant specialist.
Paul E. Sax, an infectious disease specialist at Harvard Medical School, favors such fast adoption. "There are advances in medicine that are so dramatic that they're obvious," he said. "This has to move quickly into standard of care."
But a committee convened by the American Society of Transplantation urges a go-slower approach. The 15-member panel, including Penn liver transplant specialist David S. Goldberg, last year published a review that concluded more studies are needed to fully understand the long-term risks and benefits.
"I know there are some centers that think it's the right thing to do" to offer hep C-infected organs, said lead author Josh Levitsky, a Northwestern University liver transplant specialist. "I just would encourage that it be done under research protocols so they can report the data."
Niraj Desai, director of the kidney transplant program at Johns Hopkins University, echoed that concern. "At this point," he emailed, "it is still important that patient outcomes are followed and reported so everyone in the field of organ transplantation can learn what the outcomes are in larger numbers of patients than what has so far been reported."
So far, small studies—about 100 published cases in total—have shown success with all major thoracic organ transplants, even lungs. Among the centers researching the approach besides Penn are Hopkins, Vanderbilt University, Brigham and Women's Hospital, and Massachusetts General Hospital.
Penn—the first to leap into the uncharted ethical territory starting two years ago—has eradicated hep C in 20 kidney transplant patients using the drug Zepatier, donated by Merck. Penn has done the same in 10 heart transplant patients, and is about to expand to lung transplants. So far, no transplant patients' hep C has been incurable.
Normally, hep C-infected organs are offered only to patients who already have the virus or else the precious donations are thrown away.
Using such organs would put a small but meaningful dent in the national waiting list, enabling a few thousand additional organ transplants each year, experts estimate.
However, both the number and quality of hep C infected organs has been dramatically increasing because so many young people are dying of opioid overdoses. Between 2000 and 2016, the number of infected donors more than tripled, from 181 to 661, one study found.
In a blog post for the New England Journal of Medicine, Harvard's Sax wrote that using infected organs to save people on the waiting list is "a tragic silver lining to the horrible opiate epidemic cloud."
Still, questions remain to be answered about the best treatment regimen, when therapy should begin, and how long it should last. Long term safety concerns are also unsettled.
"We don't have the kind of data we need to say whether patients (who receive infected kidneys) have more rejection," said Penn kidney transplant specialist Peter P. Reese. "We can't rule it out. It's possible there's more immunological injury with hep C infection."
One potential barrier to widespread adoption may be easing. The cost of the mainstay antiviral therapies has been falling because of competition. Merck, for example, recently slashed the list price for a course of Zepatier by 60 percent, to $21,840. That undercuts the $24,600 price of the newest entrant, Abbvie's Mavyret.
Medicare would cover antiviral treatment for transplant-induced hep C infection, the Centers for Medicare and Medicaid Services said in an email. Private insurers may also be amenable to the approach, which is more cost-effective in the long run than supportive therapies such as kidney dialysis.
"These are expensive drugs and it is a factor, but the experience of other centers that have gone down this road has been 100 percent of patients getting covered," UW cardiothoracic surgeon Jason Smith said in the press release. "We haven't heard of a center getting a denial (from an insurer) that has stood."
Experts agree that patients—in or outside of studies—must be informed of the small risk of transmitting an infection that does not respond to antiviral drug treatment and goes on to cause harmful liver inflammation.
But Robert S. Brown Jr., director of the liver transplant center at Weill Cornell Medical College, put that risk in perspective. "The failure rate of these drugs is 3 percent," he said in an article on the health website Healio. "The risk of dying on the waiting list is greater than that. It is certainly not an ethical issue in terms of risk-benefit."
Kiran Shelat, 65, of Yardley, agrees. The infected kidney he received two years ago at Penn freed him from debilitating dialysis and restored his ability to enjoy life—to exercise, hike, and travel with his wife.
"Of course, people should make an informed decision," said the recently retired civil engineer. "But at the same time, people should not fear it. That's my message."
©2018 The Philadelphia Inquirer
Distributed by Tribune Content Agency, LLC.

















