Pneumonia-causing bacteria can be spread by nose picking and rubbing
Pneumonia-causing bacteria can be spread through picking and rubbing the nose, according to new research published in the European Respiratory Journal.
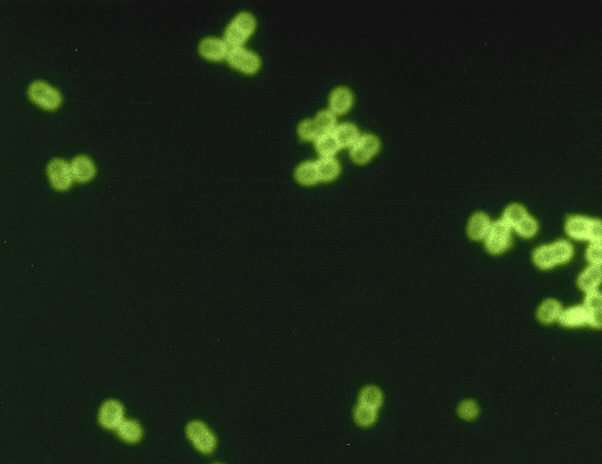
Pneumococcus, the bacteria that can cause pneumonia, is known to be spread through inhalation of airborne droplets containing the bacteria, for example in coughs and sneezes. This study is the first to show that transmission can also occur via contact between the nose and the hands after exposure to pneumococcus bacteria.
The study found that bacteria can spread at the same rate whether it is dry or wet, and at the same rate when a person picks or pokes their nose as when they rub their nose. The results suggest that ensuring good hand hygiene and keeping toys clean could help to protect young children from catching and spreading the bacteria on to other children and their elderly relatives, who may be more susceptible to infection.
Lead researcher Dr. Victoria Connor, a clinical research fellow at the Liverpool School of Tropical Medicine and Royal Liverpool Hospital, explained: "Pneumococcal infection is a major cause of death around the world, and it is estimated that it is responsible for 1.3 million deaths in children under five years annually. The elderly and people with other causes of impaired immunity, such as chronic illness, are also at an increased risk of pneumococcal infections.
"Our current understanding of the transmission of pneumococcus is poor, so we wanted to look at how it may be spread in the community. Having a clearer understanding of how the bacteria is spread will allow for better advice on how transmission can be reduced, so that there is greater prevention of pneumococcal infections."
To assess the potential for hand-to-nose contact to cause pneumococcus bacteria to spread into the nose, 40 healthy adult volunteers were randomly allocated to four groups that were exposed to pneumococcus bacteria using different hand-to-nose methods.
One group had water containing pneumococcus bacteria applied to their hands and were then asked to sniff their hands ("wet sniff"). A second group were asked to sniff air-dried pneumococcus bacteria from the back of the hand ("dry sniff"). The third and fourth group were asked to pick or poke their nose with a finger that was either exposed to wet pneumococcus bacteria ("wet poke") or exposed to air-dried pneumococcus bacteria ("dry poke").
Two different detection methods were then used to test for pneumococcus, to confirm the presence of the bacteria in the participants' noses. These included a test to see if they could grow pneumococcus bacteria from wash samples of the participants' noses (culture), and whether they could detect the presence of bacterial DNA (qPCR).
The results showed that the highest rates of bacteria spread were among participants in the "wet poke" group, followed by the "wet sniff" group.
The researchers say that participants were just as likely to get pneumococcus bacteria in their noses whether they were exposed using wet or dry samples, but the total number of bacteria passed on was higher in the wet groups; the authors suggest this may be because the air-drying process leads to the death of some bacteria.
The tests also showed that the same amount of transmission occurred when the participants poked or picked their nose as when they rubbed their nose with the back of their hand.
Dr. Connor said: "It might not be realistic to get children to stop picking, poking and rubbing their noses, and presence of the bacteria can sometimes boost the immune system of children and can reduce their chances of carrying it again later in life, so it is unclear if completely reducing the spread of pneumococcus in children is the best thing.
"But for parents, as this research shows that hands are likely to spread pneumococcus, this may be important when children are in contact with elderly relatives or relatives with reduced immune systems. In these situations, ensuring good hand hygiene and cleaning of toys or surfaces would likely reduce transmission, and reduce the risk of developing pneumococcal infection such as pneumonia."
The researchers highlight that using real people as part of the study design enabled them to test the survival of pneumococcus and the viability of transmission methods in a safe and controlled way.
Professor Tobias Welte, from Hannover University, Germany, is President of the European Respiratory Society and was not involved in the study. He said: "This pilot study is the first to confirm that pneumococcus bacteria can be spread through direct contact, rather than just through breathing in airborne bacteria.
"For clinicians, the findings reinforce the message that we must promote rigorous hand hygiene and basic infection control measures such as avoidance of sharing food, drink and mobile phones, in order to potentially reduce the transmission of respiratory bacterial pathogens such as pneumococcus. Pneumococcal vaccination is the best method for limiting the spread of S. pneumoniae in to the sinuses and lower airways, but vaccination rates are below 50% for those for whom it is recommended. To improve this is one of the major tasks for healthcare policy."
The researchers note that the bacteria samples used in the tests were given at a dose which may not represent a real-life scenario, so the results may be treated with caution. They plan to look at how pneumococcus is shed from the nose, and if hand washing reduces the spread from hand to nose.
More information: Victoria Connor et al, Hands are vehicles for transmission of Streptococcus pneumoniae in novel controlled human infection study, European Respiratory Journal (2018). DOI: 10.1183/13993003.00599-2018


















