This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Subcutaneous therapy improves inflammatory bowel disease treatment, clinical trial finds
Subcutaneous delivery of an anti-TNF inhibitor drug improved remission rates in patients with moderate-to-severe Crohn's disease and ulcerative colitis, according to recent phase 3 clinical trial results published in the journal Gastroenterology.
The findings demonstrate the efficacy and safety of an alternative maintenance therapy for patients with moderate-to-severe disease that can be self-administered in the comfort of their own home, according to Stephen Hanauer, MD, the Clifford Joseph Barborka Professor of Medicine in the Division of Gastroenterology and Hepatology and lead author of the study.
"The purpose is to give patients who are already receiving intravenous infliximab a new option, if they want to move to a subcutaneous formulation because it's more convenient, because it has less impact on quality of life, for whatever reason," Hanauer said.
Crohn's disease and ulcerative colitis (UC) are chronic inflammatory bowel diseases (IBD) of the gastrointestinal tract. Together, the diseases currently impact more than one million Americans, according to the Centers for Disease Control and Prevention.
While the symptoms are similar, Crohn's disease can cause inflammation anywhere in the digestive tract whereas ulcerative colitis only affects the large intestine. Treatment for Crohn's disease and UC is not a one-size-fits-all approach and instead is based on the current severity of the patient's disease and long-term prognosis, according to Hanauer.
For patients with mild disease, the anti-inflammatory drug mesalamine is typically administered as a baseline therapy. For moderate to severe disease, corticosteroids may help alleviate a patient's symptoms and quickly reduce inflammation but can also cause many negative side effects including increased risk of infection and bone thinning.
"Once a patient starts a steroid, the goal is to get them off it. So, the next thing is what are the therapeutic approaches that can either improve the symptoms of patients or the healing of patients who are on steroids and how to preserve the well-being of patients after steroids, because we're dealing with chronic disease," Hanauer said.
Patients who are being weaned off corticosteroids are typically given therapies including TNF (tumor necrosis factor) inhibitors that further reduce the, already, overactive immune system in the gut that leads to bowel inflammation, which causes the typical symptoms associated with IBD.
The first anti-TNF inhibitor approved by the FDA was infliximab, which is administered intravenously over the course of a two-hour infusion, and remains one of the current standard treatments for moderate-to-severe Crohn's disease and UC. In 2016, the FDA approved intravenous CT-P13—the first infliximab biosimilar drug—and in 2023, approved a subcutaneous formulation of CT-P13, which can be self-administered by patients through a skin injection.
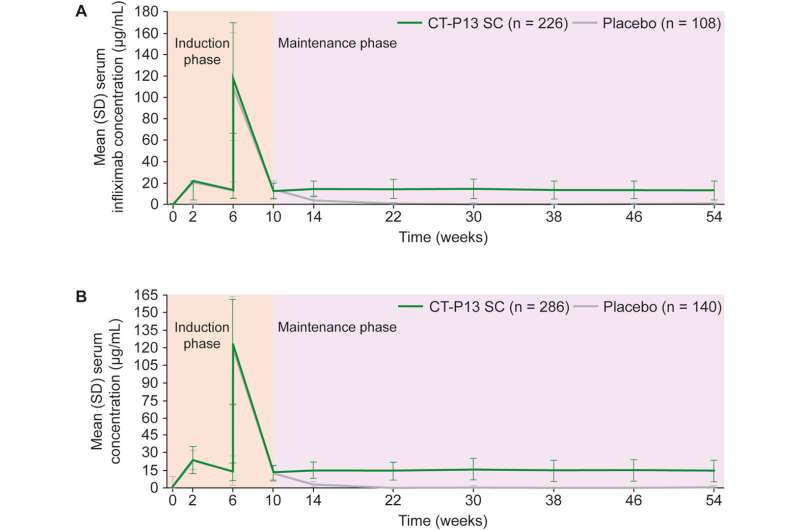
In the current study, Hanauer's team aimed to evaluate the efficacy and safety of subcutaneous CT-P13 versus placebo after CT‑P13 intravenous induction in more than 900 patients with moderate-to-severe Crohn's disease and UC who previously completed intravenous anti-TNF treatment.
All patients received CT-P13 intravenously every two weeks for the first six weeks of the trial. At week 10, patients were randomized to receive either 120 milligrams of CT-P13 subcutaneously or a placebo every two weeks until the end of 54 weeks.
In the Crohn's disease group, participants who received CT-P13 subcutaneously had higher rates of clinical remission and endoscopic response compared to those patients who received only a placebo (62.3% versus 32.1% for remission and 51.1% versus 17.9% for endoscopic response). In the UC group, clinical remission rates were also higher for patients who received CT-P13 subcutaneously compared to patients who received a placebo (43.2% versus 20.8%).
The findings demonstrate the effectiveness of subcutaneous CT-P13 as a maintenance therapy for moderate-to-severe Chron's disease and ulcerative colitis patients who previously responded to intravenous CT-P13.
"Overall, the results support CT-P13 SC as a treatment option for maintenance therapy in patients with IBD who have had an initial response to intravenous infliximab," the authors wrote.
More information: Stephen B. Hanauer et al, Subcutaneous Infliximab (CT-P13) as Maintenance Therapy for Inflammatory Bowel Disease: 2 Randomized Phase 3 Trials, Gastroenterology (2024). DOI: 10.1053/j.gastro.2024.05.006



















