Misconceptions about opioids affect pain control among cancer patients: a Malaysian survey
Misconceptions about the use of strong opioids showed to undermine optimal pain control among Asian cancer patients undergoing chemotherapy and radiotherapy according to a cross-sectional survey conducted at the Sarawak General Hospital in Malaysia.
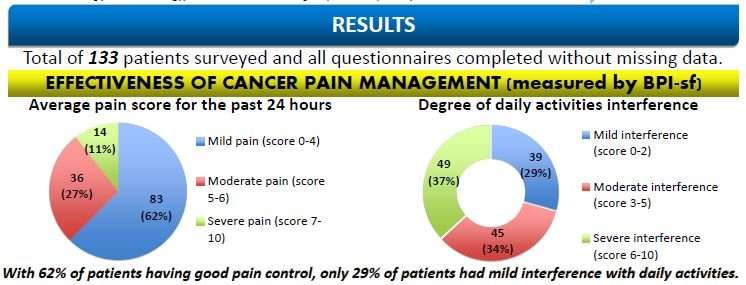
In a study to be presented at the ESMO Asia 2018 Congress, 133 patients with solid tumours across all stages treated with strong opioids were requested to rate their experience of pain during the week before the delivery of the survey questionnaire by using a visual analogue scale (VAS) from 0-10 and to self-assess the impact of pain on daily activities by completing the Brief Pain Inventory-short form (BPI-sf).
Researchers also investigated types of strong opioids used and patient-related barriers to effective cancer pain management; results were assessed by social determinants including ethnic group, religion and education level.
Overall, a good pain control was reported in 62% of survey participants (pain score < 4) treated with strong opioids usage. "Although levels of pain were improved by more than half in up to 83.5% of patients taking strong opioids —thus confirming effectiveness of these medications, some patient-related barriers still exist", said study author Dr. Voon Pei Jye of Sarawak General Hospital. "Fears that strong opioids could damage the immune system and develop addiction were observed as the most common misconceptions, in around 40% of patients. These were followed by the belief that pain could mask the monitoring of cancer progression (23.3%), perceived difficulties in managing side effects of opioids (18.05%), complaints that pain could distract doctors from treating cancer (16.5%), and a fatalistic attitude (5.3%)."
Greater barriers for pain control were found in patients with higher education levels, which may reflect pervasive misconception of opioids use in social media. Fear of harmful effects from taking opioids was observed to be more common in the Malay community, followed by Chinese and Dayak groups. "These differences may reflect some inequities in access to optimal cancer care in the state, however multiple socio-economic factors may also play a critical role in the use of opioids, thus further investigations are needed", commented Dr. Voon.
Although adequate pain relief is core to supportive care, it is still hindered by the lack of availability or accessibility to opioids in some countries, according to Prof Sumitra Thongprasert from Bangkok Hospital Chiang Mai, Thailand, co-chair of the ESMO Asia 2018 Public Policy programme. "Beliefs and other cultural issues may only partially explain a sub-optimal use of opioids analgesics, and several factors remain to be assessed including how information on benefits of these drugs is delivered by health care providers", she commented. "More importantly, access to prescription of opioids and government restrictions regarding the total amount that a patient could receive each time can significantly influence access and usage patterns among cancer patients."
Accessibility issues, costs and regulatory barriers that can limit prescribing and dispensing of opioid analgesics in low- and middle-income countries (LMICs) were firstly mapped in 2013 by the Global Opioid Policy Initiative (GOPI) conducted by ESMO with other international partners and which expanded the results of a similar survey conducted in Europe in 2010. Opioid availability was reported to be low in all 20 surveyed countries in Asia, except for South Korea and Japan, and evidence of over-regulation of opioid prescribing was found in the Asia-Pacific region that may restrict or impair access to pain relief treatments. Outcomes from this initiative also highlighted a concrete need to improve palliative care knowledge among clinicians in Asian countries.
"At present, although the availability of critical medications such as opioids, targeted medicines and immunotherapies may be potentially improved in Asia, accessibility issues will be hard to overcome in the next future due to the high costs of cancer treatments", continued Thongprasert. "Some countries across Asia/Asia-Pacific are simply not able to provide expensive medicines to local communities. Also, in countries where patients have to pay on their own for cancer treatments, high costs of medicines can be the primary reason of poor quality in cancer care."
Prof. Nathan Cherny from Shaare Zedek Medical Centre Oncology Institute, Israel, at the time co-coordinator of the Global Opioid Policy Initiative for ESMO, added: "According to the results reported in the paper published in 2013, there is agreement between the WHO, the International Narcotics Control Board, and ESMO, and the 20 international and national palliative care and oncology societies collaborating on the project, about the fact that opioid analgesic therapy is the cornerstone of cancer pain management, and that there is no economic barrier to making opioids available for this indication, and that it must be made a public health priority."
Strategies to improve accessibility to and availability of cancer medicines in LMICs will be discussed in a thought-provoking debate to be held at the ESMO Asia 2018 Congress in Singapore. "Since reducing cancer medicine costs could take some time, other potential strategies need to be assessed, such as the set-up of different pricing according to economic status; pharmaceutical companies providing Patient Access programme or Technology transfer to LMICs to manufacture their own medicines; availability of quality-assured generic and biosimilar medicines; and Compulsory Licensing of anti-cancer medicines. Beyond regulations, major barriers are likely to remain in these countries due to the rapid pace of development of new medicines, limitation of access to research projects and a lack of new technologies." added Thongprasert.
Global commitment on ensuring access to anti-cancer medicines has increased over recent years and according to ESMO President Josep Tabernero, cooperation among different stakeholders can contribute to better guiding the Asia-Pacific countries towards improving access to and availability of essential medicines, vaccines, diagnostics and medical devices.
"Overall, there is a need to adequately prioritise limited resources to clinical benefits, and collaborative efforts have resulted in new tools and approaches that can play a critical step in addressing policy issues in LMICs. One such platform is the ESMO Magnitude of Clinical Benefit Scale (ESMO-MCBS) (6,7) which can help governments to review and adjust their respective national medicine lists to ensure that they prioritise the most cost-effective ones that provide the greatest value to patients."
"Also, by facilitating education and updating of oncology professionals in the Asia-Pacific region, the annual ESMO Asia Congress, launched back in 2014, provides the arena for sharing knowledge as well as discussing and debating major challenges in oncology towards advancing the field and bringing about real and necessary change," the ESMO President concluded.
More information: Abstract 439P - 'Pain control among cancer patients receiving strong opioids and their perspective towards opioids in a developing coiuntry with a diverse multicultural background' will be presented by Daniel Lee during the Poster Display Session on Saturday, 24 November, from 18:00 to 19:00 (SGT) in the Exhibition Area. Annals of Oncology, Volume 29, 2018 Supplement 9, DOI: 10.1093/annonc/mdy426

















