Memphis study suggests transplanting Hep C-infected kidneys to uninfected donors safe
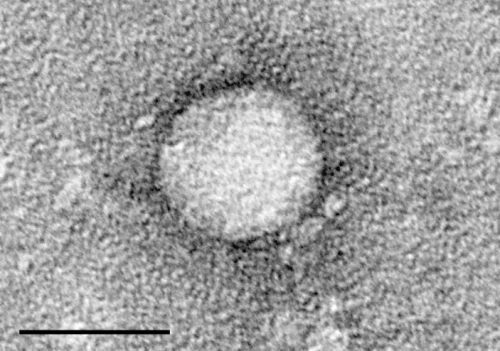
Transplantation of kidneys from Hepatitis C-infected donors to uninfected recipients is safe and can be successfully implemented as a standard of care, according to an observational study by physicians at the University of Tennessee Health Science Center and the James D. Eason Transplant Institute at Methodist University Hospital.
The practice, which has been tested in two smaller clinical trials, could greatly expand the number of kidneys available for transplantation and reduce wait times for donors, said Miklos Z. Molnar, MD, Ph.D., FEBTM, FERA, FASN, associate professor of Medicine at UTHSC, transplant nephrologist at the James D. Eason Transplant Institute, and director of the Transplant Nephrology Fellowship program at UTHSC. Dr. Molnar is the principal author of the study published by the American Journal of Transplantation.
In current practice, Hepatitis C-infected kidneys are transplanted only to patients already infected with the disease, Dr. Molnar said. The number of these available kidneys greatly exceeds the infected population. As a result, up to 1,000 Hepatitis C-infected kidneys or more are discarded annually.
"Our thought was using these kidneys, which are usually pretty good, other than the Hepatitis C," he said.
The Memphis team began its study in March 2018. To date, more than 80 uninfected recipients have received Hepatitis C-infected kidneys. The paper cites 53 patients, since the remainder are too soon after transplant to evaluate fully.
All patients consented to the surgery in three separate steps, after being made aware that by receiving an infected kidney, they would be infected with Hepatitis C. All were successfully transplanted, and after receiving 12 weeks of antiviral therapy, show no signs of Hepatitis C and are considered cured. "We did not lose any patients, but there were some unexpected complications," Dr. Molnar said. High volume of BK virus, common after transplantation and generally treatable, was evidenced in a number of the recipients.
While this factor will demand further research, Dr. Molnar said the study results are positive for patients in need of transplant. "These people would not get this offering (a transplant) without these kidneys," he said. "If you're willing to accept these kidneys, the waiting time can go down by two years."
The five-year survival rate on dialysis is 50 percent, Dr. Molnar said. "We are losing 10 percent of the patients every year on dialysis."
Dr. Molnar said the study indicates that transplantation of Hepatitis C-infected kidneys to Hepatitis C-negative recipients has potential to become the standard of care in the United States. "Otherwise, the patients would be on dialysis and die," he said. "These patients have good kidney graft function. The transplantation of Hep C-infected kidney to non-Hep C-infected recipients can be done and should be done."
Director of the Transplant Institute James Eason, MD, said, "This is a landmark paper outlining a novel approach to using kidneys, that would otherwise be discarded, to save more lives."
More information: Miklos Z. Molnar et al, Transplantation of kidneys from hepatitis C–infected donors to hepatitis C–negative recipients: Single center experience, American Journal of Transplantation (2019). DOI: 10.1111/ajt.15530














