Saving patients an unnecessary procedure: The 5-SENSE score can predict who will not benefit from stereo-electroencephy
A new study from The Neuro (Montreal Neurological Institute-Hospital) and eight collaborating international epilepsy centers has developed a simple web-based application clinicians can use to predict which patients will not benefit from an invasive diagnostic work-up, preventing unnecessary, invasive procedures, saving time for patients and the clinical team, and freeing up overburdened health resources.
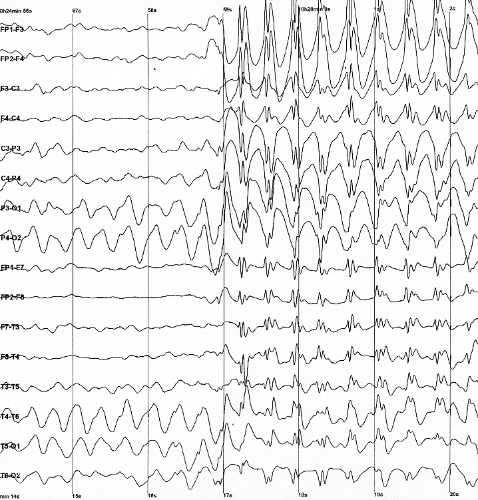
Surgery is the only option to cure seizures inpatients with drug-resistant epilepsy. In evaluating patients for surgery, clinicians have to pinpoint what brain region the seizures are coming from. The way to do this in patients with more complex epilepsy is through stereo-electroencephalography (SEEG), a technique by which a surgeon implants electrodes into the brain to find the source of the seizures.
SEEG is an invasive procedure that requires a one-to-two-week hospital stay and comes with risk of infection, bleeding and stroke in 0.5-2 percent of procedures. Furthermore, in up to 42 percent of case series, SEEG does not result in an epilepsy surgical intervention as no focal epileptic focus can be identified. To reduce the amount of people undergoing an unnecessary SEEG, researchers studied epilepsy patients to determine if a series of non-invasive tests could predict which patients would not benefit from SEEG.
The team followed 128 patients at The Neuro who had SEEG, analyzing their demographic, clinical, electroencephalography, neuroimaging, and neuropsychological data. They developed a regression model based on different modalities, called the "5-SENSE-score", that differentiated patients whose SEEG identified a defined seizure source from those that did not. They then validated this score on a larger cohort of 207 patients from nine different tertiary epilepsy centers, finding that it reliably predicted the patients in whom SEEG was unable to identify a focal seizure onset zone.
"Many epilepsy centers face the challenging decision of whether a patient should undergo implantation for identifying a focal-seizure onset zone," says Dr. Birgit Frauscher, neurologist at The Neuro and the study's senior author. "The 5-SENSE-score provides an easily applicable tool to guide clinicians in predicting patients where SEEG is unlikely to identify a focal seizure onset zone. Patients unlikely to benefit from this invasive and resource-intensive procedure can then be identified earlier, avoiding unnecessary burden on patients and overutilization of hospital resources."
This study is published in the Journal of the American Medical Association on Dec. 6, 2021.
More information: Development and Validation of the 5-SENSE Score to Predict Focality of the Seizure-Onset Zone as Assessed by Stereoelectroencephalography, Journal of the American Medical Association (2021). DOI: 10.1001/jamaneurol.2021.4405



















