Long COVID case study: Recovery process for impaired hormone secretion
Recently, "Long COVID" is becoming a significant medical issue worldwide. It refers to a variety of symptoms that persist over an extended period after the patient has recovered from a novel coronavirus infection (COVID-19). In many cases, it is unclear what causes Long COVID symptoms, and there is insufficient information regarding recovery time.
To help address this, a research collaboration between Kobe Graduate School of Medicine and Hyogo Prefectural Kakogawa Medical Center report a 15-month case study on a patient's recovery from impaired adrenocorticotropic hormone secretion brought on by novel coronavirus infection. The research team included Professor Ogawa Wataru and Assistant Professor Yamamoto Masaaki (both of the Division of Diabetes and Endocrinology, Department of Internal Medicine, Kobe University Graduate School of Medicine), and Dr. Iida Kenji (Head of the Division of Diabetes and Endocrinology at Hyogo Prefectural Kakogawa Medical Center).
This case study provides an example of the recovery period for a hormone secretion disorder, one of the widely reported aftereffects of COVID-19. This information will hopefully help people whose quality of life (QoL) has declined due to Long COVID.
This case study was published in the Endocrine Journal on July 14.
Novel coronavirus can cause respiratory illness, in particular pneumonia. However, it has been reported that novel coronavirus infection can also affect various other parts of the body beyond the respiratory system, including the heart and blood vessels, the digestive organs and liver, the nervous system, muscles and bones. Previous research has reported that impairment of the endocrine organs (pituitary gland, thyroid, pancreas, adrenal glands, and testes) is accompanied by decreased hormone secretion.
Case study
After having symptoms such as fever and breathing difficulties for over one week, the subject of this case study took a PCR test, which came back positive. He was subsequently hospitalized for treatment but his breathing difficulties significantly worsened due to pneumonia and he had to be put on a respirator. Through treatment (including anti-viral medication) the patient gradually recovered from respiratory failure to the point where he could be taken off mechanical ventilation. However, 10 days or so after being taken off mechanical ventilation, his blood pressure suddenly dropped and the test results showed that ACTH secretion was severely impaired. Administration of ACTH rapidly restored the patient's blood pressure.
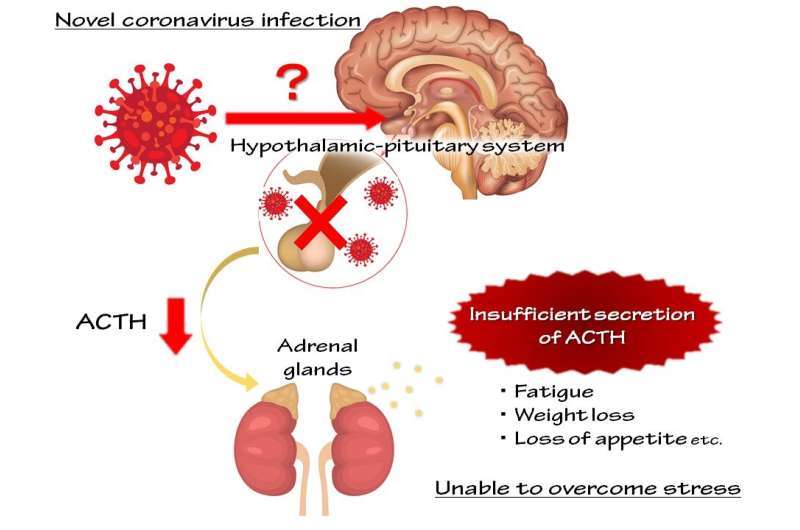
A detailed hormone test showed that hypothalamic-pituitary system impairment had caused a decrease in growth hormone secretions as well as ACTH. The patient was given ACTH replacement therapy, which ameliorated hormone secretion. After a year and a half, hormone levels had returned to normal and replacement therapy was no longer necessary.
There have been many reports of endocrine organ impairment leading to decreased hormone secretion in patients during treatment for novel coronavirus or post-infection. However, this is the first reported case study in the world to track the recovery process and follow up on a patient with this particular long COVID symptom.
The significance of these findings and further developments
Although many surveys are being conducted on Long COVID in countries all over the world, its pathology remains elusive. It is also not fully understood how long these symptoms persist.
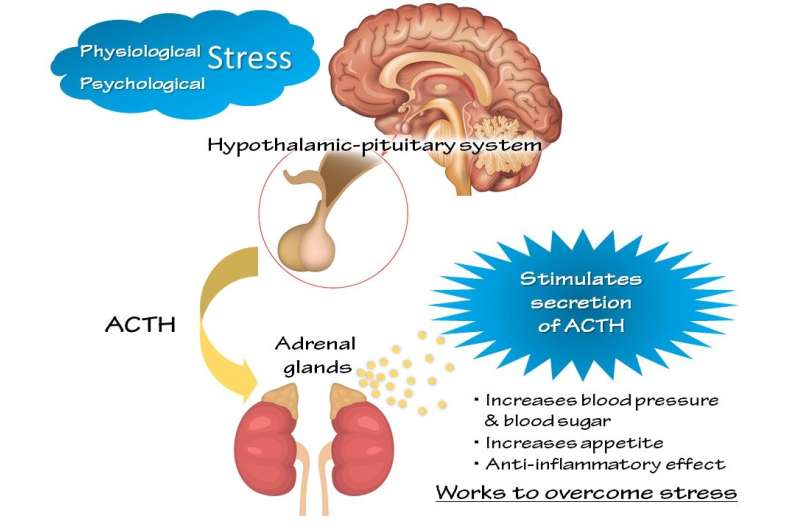
In this case study, ACTH was one of the hormones with impaired secretion. ACTH is normally secreted by the body in response increased physiological or psychological stress. However, the body is unable to fight effectively against stress when not enough of this hormone is secreted. If there is a high level of secretion impairment, this causes severe, life threating symptoms. On the other hand, slight impairment causes non-specific symptoms such as becoming tired easily, a lack of energy, and low mood. Therefore adrenal insufficiency is easily overlooked in routine medical examinations.
Previous research has reported that decreased ACTH secretion as an aftereffect of novel coronavirus infection occurs at a frequency of 16.2%; therefore, this case study is not a rare example. Many of the Long COVID symptoms resemble those of adrenal insufficiency; therefore it is highly probable that among novel coronavirus aftereffects, the lighter symptoms of adrenal insufficiency are being overlooked.
It is currently unclear how long the aftereffects of novel coronavirus infection typically last. There are currently people who are suffering from Long COVID with no clear end in sight. This case study, which shows the recovery process for one of the aftereffects, is especially significant for these people.
Next, Assistant Professor Yamamoto and the team plan to work with hospitals nationwide to conduct surveys on hormone secretion levels in patients who are experiencing novel coronavirus aftereffects.
More information: Kai Yoshimura et al, Coexistence of growth hormone, adrenocorticotropic hormone, and testosterone deficiency associated with coronavirus disease 2019: a case followed up for 15 months, Endocrine Journal (2022). DOI: 10.1507/endocrj.EJ22-0108















